Hyponatremia Risk Calculator
Assess Your Risk
This tool helps you understand your risk of severe hyponatremia (low sodium) when taking certain medications. Risk increases with age, gender, and duration of use.
Low sodium isn’t just a lab number-it can turn a healthy person into someone confused, seizing, or unresponsive in a matter of days. And it’s often not from dehydration or kidney disease. More often, it’s from a medication you started last month. Hyponatremia-serum sodium below 135 mmol/L-is common. But when it drops below 120 mmol/L? That’s a medical emergency. The brain swells. Symptoms hit fast. And if you don’t recognize them, the damage can be permanent.
What Medications Cause Severe Hyponatremia?
It’s not just one drug. It’s a group. The biggest culprits? Diuretics like hydrochlorothiazide, SSRIs like sertraline and citalopram, and antiepileptics such as carbamazepine and oxcarbazepine. These aren’t rare or experimental drugs. They’re among the most prescribed in the UK and US. A 2023 study from the University of California found that nearly 1 in 50 hospital admissions for hyponatremia came from someone taking one of these. SSRIs are especially tricky. People start them for anxiety or depression. They feel a little nauseous at first. Maybe a headache. Their doctor says, "That’s normal." But if sodium drops 0.8 mmol/L per day-something that happens in 40% of cases within 10 days-it’s not just side effects. It’s a chemical imbalance in the brain. The drug triggers SIADH-syndrome of inappropriate antidiuretic hormone secretion. The kidneys hold onto water. Blood gets diluted. Sodium crashes. Other offenders include ACE inhibitors, some NSAIDs, and even MDMA. But the real danger isn’t the drug itself. It’s the lack of monitoring. No one checks sodium levels after starting these meds. Not in primary care. Not in pharmacies. Not until someone collapses.How Fast Does It Happen?
This isn’t a slow decline. In older adults, especially women over 65, sodium can drop fast-sometimes 1 mmol/L per day. Within 5 to 10 days, symptoms appear. Confusion. Nausea. Headache. Then, seizures. Coma. Death. Data from the Merck Manual shows 68% of severe cases involve confusion. That’s not just "feeling off." It’s forgetting names, mixing up days, not recognizing family. StatPearls reports that when sodium falls below 115 mmol/L, seizures occur in 22% of patients. And if it stays that low for more than 48 hours without correction, mortality hits 37%. The worst part? Many of these cases are misdiagnosed. On patient forums, 68% report being told they had the flu, anxiety, or early dementia. A nurse on Reddit shared a case: a 72-year-old man started sertraline. He got headaches. His GP said, "It’s just adjusting." Ten days later, he had a grand mal seizure. Sodium: 118 mmol/L. He spent five days in ICU.Why Are Older Adults and Women at Higher Risk?
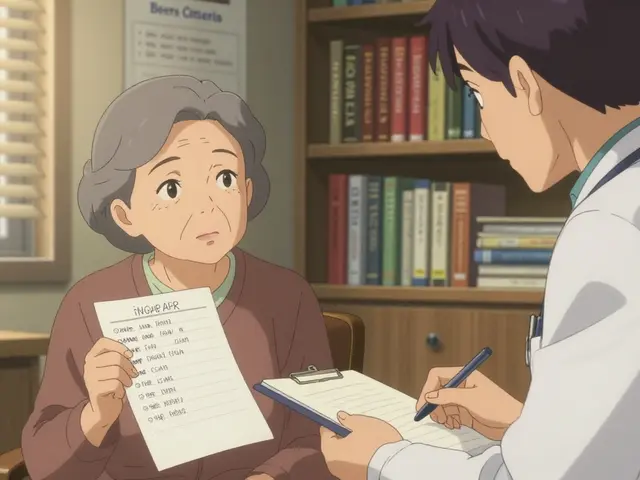
Sixty-one percent of severe medication-induced hyponatremia cases happen in people over 65. Why? Kidneys don’t handle water the same way. Hormonal changes make them more sensitive to SIADH. Women are affected in 57% of cases-partly due to lower body weight, hormonal differences, and higher rates of depression and SSRI use. A 2023 study in the American Geriatrics Society guidelines found that people over 65 have 2.7 times the baseline risk. That’s not a small increase. It’s a red flag. If you’re prescribing an SSRI or diuretic to a 70-year-old woman, you should be checking sodium before day 7. Yet, only 47% of community clinics do routine screening. Academic hospitals? 82%. The gap is dangerous.
What Are the Real Signs to Watch For?
Don’t wait for seizures. Look for the early signs:- Unexplained nausea or vomiting (not from food)
- Headaches that won’t go away with painkillers
- Feeling unusually tired or sluggish
- Confusion-forgetting appointments, mixing up words, not recognizing familiar places
- Muscle cramps or weakness
- Loss of appetite
How Is It Treated?
Treatment isn’t simple. You can’t just give salt. Too fast, and you risk osmotic demyelination syndrome-a rare but devastating condition where the brain’s protective coating gets destroyed. That happens in 9% of cases where sodium is corrected too quickly. The goal? Raise sodium slowly. No more than 6-8 mmol/L in the first 24 hours. In hospitals, that means IV fluids with controlled saline, sometimes with drugs like tolvaptan (Samsca), approved by the FDA in November 2023 for this exact use. Tolvaptan helps the body flush out water without losing sodium, and clinical trials show it cuts correction time by 34%. For mild cases, stopping the drug may be enough. In 78% of cases, sodium returns to normal within days of discontinuing the offending medication. But here’s the catch: if the drug is essential-like an SSRI for severe depression-you can’t just stop it. That’s why recurrence rates hit 33% for SSRI users, compared to 12% for diuretic users, where alternatives exist.How to Prevent It
Prevention is simple. But it’s not happening.- Check sodium before starting high-risk meds: SSRIs, diuretics, carbamazepine.
- Check again at day 7, and again at day 14.
- For patients over 65, check every 3-5 days during the first month.
- Ask: "Has the patient had headaches, nausea, or confusion since starting this?" Don’t assume it’s "just side effects."
- Pharmacists: flag interactions. One Mayo Clinic patient said their pharmacist caught a dangerous combo before they even filled the prescription. That saved them.

What’s Changing in 2025?
The tide is turning. AI is helping. Mayo Clinic’s pilot algorithm analyzes EHR data-meds, age, lab trends-and predicts hyponatremia risk 72 hours before symptoms appear. Accuracy? 87%. That’s not science fiction. It’s in use now. More hospitals are adopting the European Hyponatremia Network’s algorithm. It’s 89% accurate at identifying medication causes when used within 24 hours of symptom onset. And the National Hyponatremia Foundation is pushing for mandatory sodium checks within 30 days of starting high-risk drugs. The cost of inaction? $473 million a year in the US alone. Thousands of preventable hospitalizations. Permanent brain damage in people who just needed an antidepressant.What Should You Do If You’re on One of These Drugs?
If you’re taking an SSRI, diuretic, or antiepileptic:- Ask your doctor: "Have you checked my sodium since I started this?"
- If you’ve been on it more than 10 days and feel off-headache, nausea, confusion-get a blood test. Don’t wait.
- Keep a symptom log: note when you feel different, even if it seems minor.
- If you’re over 65 or female, insist on monitoring. Your risk is higher.
- Don’t stop your medication without talking to your doctor-but don’t ignore symptoms either.
Can medication-induced hyponatremia be reversed?
Yes, if caught early. Sodium levels can return to normal within days after stopping the drug or with proper medical treatment. But if correction is too fast, it can cause brain damage. Slow, controlled correction under medical supervision is key.
Which drugs are most likely to cause low sodium?
Diuretics (like hydrochlorothiazide), SSRIs (like sertraline and citalopram), and antiepileptics (especially carbamazepine and oxcarbazepine) are the top culprits. Less common but still risky are ACE inhibitors, NSAIDs, and some antidepressants like MAOIs.
How long does it take for symptoms to appear after starting a drug?
Symptoms usually develop between 1 and 4 weeks after starting the medication. But in some cases-especially in older adults-they can appear as early as 5 to 10 days. Sodium can drop by 0.8 mmol/L per day, so symptoms can escalate quickly.
Is hyponatremia from medications more dangerous than other causes?
It’s not necessarily more dangerous, but it’s more sudden. Unlike slow-developing hyponatremia from heart or kidney disease, medication-induced cases often cause rapid neurological decline. The brain doesn’t have time to adapt. That’s why confusion and seizures happen faster-and why early detection saves lives.
Should I get my sodium checked if I’m on an SSRI?
Yes, especially if you’re over 65, female, or have other risk factors. The first check should be within 7 days of starting the drug, and again at 14 days. Many doctors don’t order this routinely-but it’s one of the easiest ways to prevent a medical emergency.
Can I still take my medication if I have low sodium?
It depends. If the drug is essential-like an SSRI for severe depression-your doctor may keep you on it while managing sodium levels with fluid restriction or medications like tolvaptan. But if alternatives exist, switching may be safer. Never stop medication without medical advice.





Jay Ara
December 26, 2025 AT 02:21just started sertraline last week and been getting these weird headaches
thought it was stress but now im kinda scared
gonna call my doc tomorrow to check sodium
josue robert figueroa salazar
December 26, 2025 AT 21:59another case of doctors treating symptoms instead of causes
we’re just throwing pills at people and hoping they dont die
david jackson
December 27, 2025 AT 18:46imagine being prescribed an antidepressant and then having your brain slowly drown in its own fluid because no one thought to check a basic blood panel
its not just negligence its a systemic failure
we have the tools we have the data we have the guidelines
but the system is built on inertia and convenience
and people like you and me are the collateral damage
and dont even get me started on how pharmacies arent trained to flag this
theyre cashiers with stethoscopes pretending theyre clinicians
its terrifying
jesse chen
December 29, 2025 AT 16:57thank you for writing this-it’s so important.
My mom was misdiagnosed with dementia after starting hydrochlorothiazide-she was just 68.
Turned out her sodium was 119. She spent a week in ICU.
Now she’s fine, but her memory hasn’t fully come back.
Please, if you’re on these meds-get tested. It’s a 5-minute blood draw.
It could save someone you love.
Joanne Smith
December 30, 2025 AT 13:44oh great. another ‘your brain is melting’ post from someone who clearly hasn’t met a real doctor
next you’ll tell me caffeine causes brain rot
and that every headache is hyponatremia waiting to happen
lol
people panic over lab values like they’re horoscopes
and then wonder why medicine is so broken
Prasanthi Kontemukkala
January 1, 2026 AT 12:28i understand the fear but let’s not turn every side effect into a crisis
many people take SSRIs for years without issue
the key is awareness-not alarm
if you feel off, talk to your doctor
don’t panic, don’t quit cold turkey
but also don’t ignore it
balance is everything
Alex Ragen
January 3, 2026 AT 07:35the real tragedy isn’t hyponatremia-it’s the epistemological collapse of modern medicine
we’ve reduced the human body to a series of pharmacological variables
and in doing so, we’ve abandoned the art of listening
the brain doesn’t just react to sodium-it reacts to meaning, to context, to silence
yet we measure, we label, we prescribe-and call it care
what have we become?
Lori Anne Franklin
January 5, 2026 AT 06:48my cousin had a seizure from carbamazepine and they thought it was a stroke
thank god her pharmacist caught it before she went to the ER
she’s fine now but it took 3 weeks to get anyone to listen
please if you’re on these meds-keep a journal
write down every weird feeling
even if it seems dumb
your future self will thank you
wendy parrales fong
January 6, 2026 AT 21:19you’re right to be scared
but you’re not alone
and you’re not broken
your body is just telling you something’s off
listen to it
ask for the test
you deserve to feel safe in your own skin
and if your doctor won’t help? find someone who will
you’re worth the effort
Jeanette Jeffrey
January 8, 2026 AT 08:44you people are hilarious
you take a pill for sadness and then act like your brain is a ticking bomb
get a hobby. go outside. stop Googling symptoms at 3am
you’re not dying-you’re just anxious
and now you’ve convinced yourselves you’re victims of Big Pharma
congrats. you’ve won the internet.