When you’re told you’re allergic to penicillin, it hits like a plot twist in a medical drama. You think you’ll just avoid one or two medicines, but then you discover amoxicillin is off the table—plus a whole umbrella of drugs you had no reason to care about before. So what’s next when your go-to is a big no from your immune system? Luckily, doctors aren’t left scrambling. Modern medicine hands out some great backups, and it’s not about rolling the dice. This stuff is mapped out down to the molecules.
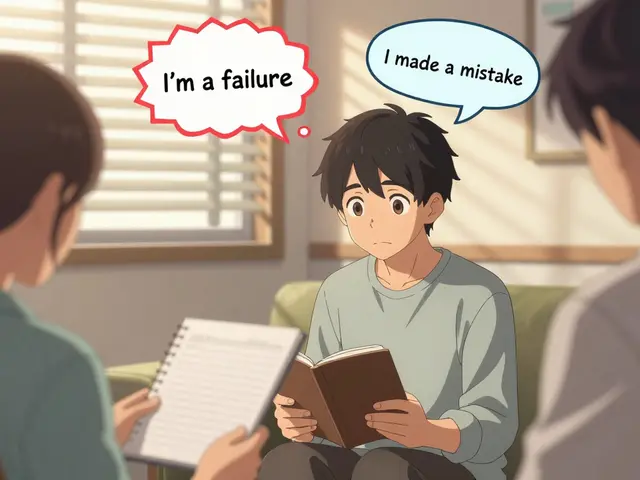
Understanding Penicillin Allergies and Cross-Reaction Myths
First off, let’s bust a myth: not every “penicillin allergy” is deadly. Around 90% of people who think they’re allergic actually aren’t—maybe it was a rash as a toddler from a virus rather than the drug, or maybe the reaction was unrelated. Still, the risk is real for some, and you don’t want to gamble. What’s wild is that avoiding amoxicillin means you also dodge every “beta-lactam” antibiotic: think penicillins like ampicillin, oxacillin, and, yes, amoxicillin itself. But what about cephalosporins? The story is murkier. Decades ago, doctors thought there was a high risk if you jumped from penicillin to cephalosporins, but more recent research shows most forms are probably fine, especially newer “generations.” This risk is trickier if your allergy was severe, like anaphylaxis.
You might be wondering: is there a cheat sheet for all this? Here are some clues. If you had a mild rash, many doctors might cautiously consider a cephalosporin so you can avoid the heavy-hitters. But if your reaction involved trouble breathing, hives all over, or needed an EpiPen—forget it. For those folks, doctors rely more on other classes like macrolides and fluoroquinolones. And if you’re pregnant or under age 12, the choices narrow, since not every alternative plays nice with babies, ears, or teeth.
Why not just test if you really have a penicillin allergy? Skin testing is an option, but most people don’t get it unless antibiotics are truly limited. For the rest of us, we stick to safer alternatives and muscle through.
Macrolides: The Go-To Substitute and What They Handle Best
Macrolides are the bread and butter backup for so many common infections. Drugs like azithromycin (that’s Zithromax, aka the “Z-pack”), clarithromycin, and erythromycin cover quite a bit. These are lifesavers for things like respiratory infections, strep throat (when penicillin isn’t safe), and some skin woes. Their magic trick? They zap bacteria by halting their protein production—sort of like cutting the power to a factory.
Here’s the catch: macrolides don’t hit every bug. Some bacteria have grown resistant, especially to erythromycin, which is why azithromycin tends to get top billing. Azithromycin is a favorite for sinus infections, bronchitis, and “walking pneumonia” (mycoplasma), but it doesn’t perform as well against more serious strep or staph infections. Doctors are also cautious when prescribing these if you’re dealing with a severe pneumonia or skin abscess; they’ll check the bug involved before reaching for these meds.
- Azithromycin: Mild to moderate respiratory infections, certain ear infections, uncomplicated skin infections, and sexually transmitted infections like chlamydia.
- Clarithromycin: Sinusitis, bronchitis, some gastrointestinal infections (like H. pylori), and some skin infections.
- Erythromycin: Rarely first choice, but used for whooping cough (pertussis) and people allergic to both penicillins and cephalosporins.
Macrolides are usually super well-tolerated. Their main side effect is sometimes stomach upset or, weirdly, metallic taste in your mouth. One sneaky thing: they can mess with the electrical activity in your heart, so doctors avoid them if you have certain heart conditions or take medications like amiodarone.

Fluoroquinolones and Cephalosporins: Expanding Your Toolbox With Caution
Sometimes you need something even stronger or different than a macrolide. Enter fluoroquinolones and cephalosporins. These drugs are workhorses for everything from urinary tract infections to pneumonia and skin infections (and in the hospital, you see them used even more often).
- Ciprofloxacin (Cipro) and levofloxacin (Levaquin) are the two fluoroquinolones you’ll run into most. They smash hard-to-treat infections—think complicated urinary tract infections, some severe respiratory bugs, and even certain food poisoning cases. But these drugs come with baggage. FDA warnings plaster their labels thanks to rare—but real—risks: tendon rupture, nerve damage, high blood sugar swings, and even mental health effects. They aren’t handed out for little earaches anymore.
- Cephalosporins feel a little less wild west than fluoroquinolones. Newer generations (like cefuroxime, cefdinir, ceftibuten, and cefpodoxime) almost never trigger a reaction in penicillin-allergic folks because their side chains—where the immune system “sees” most of the drug—are different. Older ones (like cephalexin and cefazolin) are closer in shape to penicillins, but the real risk is a lot smaller than once thought. If you had a life-threatening allergy, your doc might steer clear, but with milder reactions, you might still get these with a little supervision in the clinic.
Thinking about what infection you have actually matters. Here’s a quick chart for the real world:
- Ear Infections: Azithromycin, clarithromycin, cefdinir, cefuroxime
- Sinus Infections: Azithromycin, levofloxacin, cefuroxime
- Urinary Tract Infections: Nitrofurantoin (if kidneys are healthy), ciprofloxacin, levofloxacin, ceftibuten
- Strep Throat: Azithromycin (five days vs ten days for most antibiotics), clarithromycin (ten days), rare cases of cephalosporin
- Pneumonia: Levofloxacin, azithromycin, ceftriaxone + azithromycin (in hospital), moxifloxacin
- Skin Infections: Clindamycin, doxycycline (if not pregnant or a child!), cephalexin (only with careful monitoring), linezolid for MRSA suspected
If you want more nitty-gritty details, check out this more detailed breakdown here: alternatives for amoxicillin. It’s a good crash course if you want help navigating pharmacy shelves without rolling the dice.
Doctors weigh all kinds of stuff when picking an antibiotic. Your age, health, whether you’re pregnant, allergies, any past side effects, and—honestly—where you live. Resistance rates matter more than brand names. In my neighborhood, for example, azithromycin barely dents strep throat, but one town over, it’s still king. Your doc’s seen this play out hundreds of times, so listen to what they say—even if it means skipping a “Z-pack” because it’s just not strong enough for your kind of cough.
If you get an antibiotic prescription as an alternative for penicillin, here’s a checklist before popping your first pill:
- Double-check the pharmacy label for your listed allergies—they should always match your chart.
- Ask if side effects of the new drug are different than what you might expect from amoxicillin.
- Find out if you should take it with food. (Erythromycin is nasty on an empty stomach, trust me.)
- Finish your whole course, unless reactions crop up—stopping early is how resistance builds.
- If you feel weird (tight chest, trouble swallowing, rash), call the doctor or go to urgent care. Don’t try to "tough it out."
All this can sound like a lot, but keep in mind the whole system is actually built for safety. You’re not going to end up in that 1950s scenario where penicillin is the only option. Today, your pharmacist and doctor have entire books (literally called "antibiograms") showing which drugs work best for every infection in your zip code.
Oh, and don’t go digging in that leftover “emergency” stash from your last illness. If you’re anything like my wife Kara, you think keeping one or two stray pills for a rainy day is a smart move—but mixing and matching antibiotics from your medicine cabinet is a recipe for disaster. Bacteria aren’t playing around, and neither should we.






Charity Peters
July 24, 2025 AT 11:17Just took azithromycin last week for a sinus thing. Tasted like metal and my stomach hated me, but it worked. Glad I didn't get amoxicillin.
Sarah Khan
July 26, 2025 AT 02:35It's wild how we treat allergies like they're static labels when biology is always whispering changes. I had a rash at six, got labeled penicillin-allergic, and spent 20 years avoiding half the pharmacy. Turned out I was never allergic-just had a virus. Skin test finally cleared me. Now I take amoxicillin like it's candy. Doctors still treat the label, not the person. We need to stop letting old charts dictate modern biology. It's not just medical-it's philosophical.
Kelly Library Nook
July 27, 2025 AT 04:18It is imperative to note that the assertion regarding cephalosporin cross-reactivity is not universally supported by clinical guidelines. The 2010 JAMA study cited by the author is outdated; the 2020 IDSA guidelines explicitly state that third-generation cephalosporins present a negligible risk in penicillin-allergic patients, even those with prior anaphylaxis, provided there is no IgE-mediated history. Failure to distinguish between IgE-mediated and non-IgE-mediated reactions constitutes a critical clinical error. This article, while accessible, lacks the rigor expected of evidence-based medicine.
Faye Woesthuis
July 27, 2025 AT 23:50If you're still taking azithromycin for everything, you're part of the problem. Antibiotic overuse is why we're in this mess. Stop being lazy and get tested.
raja gopal
July 29, 2025 AT 07:01I'm from India and we don't always have access to fancy tests. But I've seen my mom take cefdinir after being told she was allergic-no issues. Sometimes the best medicine is trust in your doctor, not fear of labels. We need more stories like this, not just warnings.
Samantha Stonebraker
July 30, 2025 AT 16:56There’s something deeply human about how we cling to medical labels like they’re tattoos. I used to panic every time a nurse asked about penicillin-even though I never had a real reaction. It wasn’t until I read about the 90% myth that I stopped feeling like a walking liability. You’re not broken because you’re allergic. You’re just part of a system that’s still learning how to listen. Thank you for writing this. It felt like someone finally turned on the lights in a room I’d been stumbling through for years.
Kevin Mustelier
July 31, 2025 AT 08:04So… macrolides = good? Fluoroquinolones = bad? Cephalosporins = maybe? 😅
TL;DR: Don’t trust your doctor. Don’t trust your label. Just take whatever’s handed to you and hope for the best. 🤷♂️
Keith Avery
August 2, 2025 AT 03:39Let’s be real-this article is just a marketing brochure for Big Pharma’s second-tier antibiotics. Azithromycin? Overprescribed. Fluoroquinolones? Dangerous. Cephalosporins? Still risky. The real solution isn’t swapping one drug for another-it’s developing targeted antimicrobials that don’t destroy your microbiome. But that’s too expensive, so we keep recycling the same flawed options. This isn’t medicine. It’s damage control.
Luke Webster
August 3, 2025 AT 02:04I grew up in the U.S. but spent years in rural India where antibiotics were sold over the counter. No tests, no charts, just a pharmacist’s guess. I saw people get better with cefixime when penicillin wasn’t available. I also saw people get worse because they took leftover pills. This piece nails the balance: respect the science, but don’t ignore context. Where you live changes what’s safe. Knowledge isn’t just power-it’s survival.
Natalie Sofer
August 4, 2025 AT 01:44i just wanted to say thank you for this post. i’ve been scared of antibiotics for years after a bad reaction as a kid. i didn’t know i could get tested. i’m gonna call my doctor tomorrow. i hope it’s not too late 😅
Tiffany Fox
August 5, 2025 AT 04:14Finish the whole course. Even if you feel fine. Trust me. I learned this the hard way.
Rohini Paul
August 7, 2025 AT 02:10My cousin in Delhi got ceftriaxone for pneumonia after penicillin reaction-no problem. But her doctor checked her heart first. That’s the real key: context. Not fear. Not labels. Just smart checks.
Courtney Mintenko
August 8, 2025 AT 21:32They say ‘90% aren’t allergic’ but what if you’re the 10% who almost died? You think your trauma doesn’t matter because some study says ‘it’s probably fine’? 🤡
My EpiPen is still in my purse. I don’t care what your ‘recent research’ says.
Sean Goss
August 9, 2025 AT 01:25There’s no such thing as a ‘mild’ penicillin allergy. That’s a misnomer. If you had a reaction, you’re IgE-sensitized. The cephalosporin cross-reactivity data is statistically insignificant in real-world practice. The FDA black box warnings on fluoroquinolones exist for a reason: they’re molecular wrecking balls. Macrolides? Fine for bronchitis, useless for pneumonia. This article is a superficial gloss on a complex pharmacological landscape. You need a clinical pharmacist, not a blog.
Khamaile Shakeer
August 9, 2025 AT 15:10Bro… why are we even using antibiotics for sinus infections? 😑
Most are viral. We’re just training superbugs. 🤦♂️💊
Stop prescribing. Start educating.
Suryakant Godale
August 10, 2025 AT 02:05It is essential to underscore that the clinical decision-making process regarding antibiotic substitution must be individualized and informed by detailed patient history, microbiological data, and local resistance patterns. The generalizations presented herein, while accessible, risk fostering therapeutic complacency. A structured allergy evaluation, including skin testing and graded challenge when appropriate, remains the gold standard. Without such diligence, we perpetuate the very iatrogenic harm we seek to prevent.
John Kang
August 11, 2025 AT 02:20My kid had a rash on amoxicillin at age 3. We did the skin test at 14. Turned out fine. Now she takes penicillin for every infection. I wish we’d done it sooner. Don’t wait. Get tested.