Most people with diabetes rely on insulin to stay alive. But for a small number, the very thing that keeps them healthy can trigger a dangerous reaction. Insulin allergies are rare - affecting about 2.1% of insulin users - but they can be serious, even life-threatening. If you’ve noticed swelling, itching, or trouble breathing after an injection, you’re not imagining it. This isn’t just a bad reaction to the needle. It’s your immune system responding to insulin or one of its additives. And ignoring it could cost you more than comfort - it could cost you your health.
What Does an Insulin Allergy Actually Look Like?
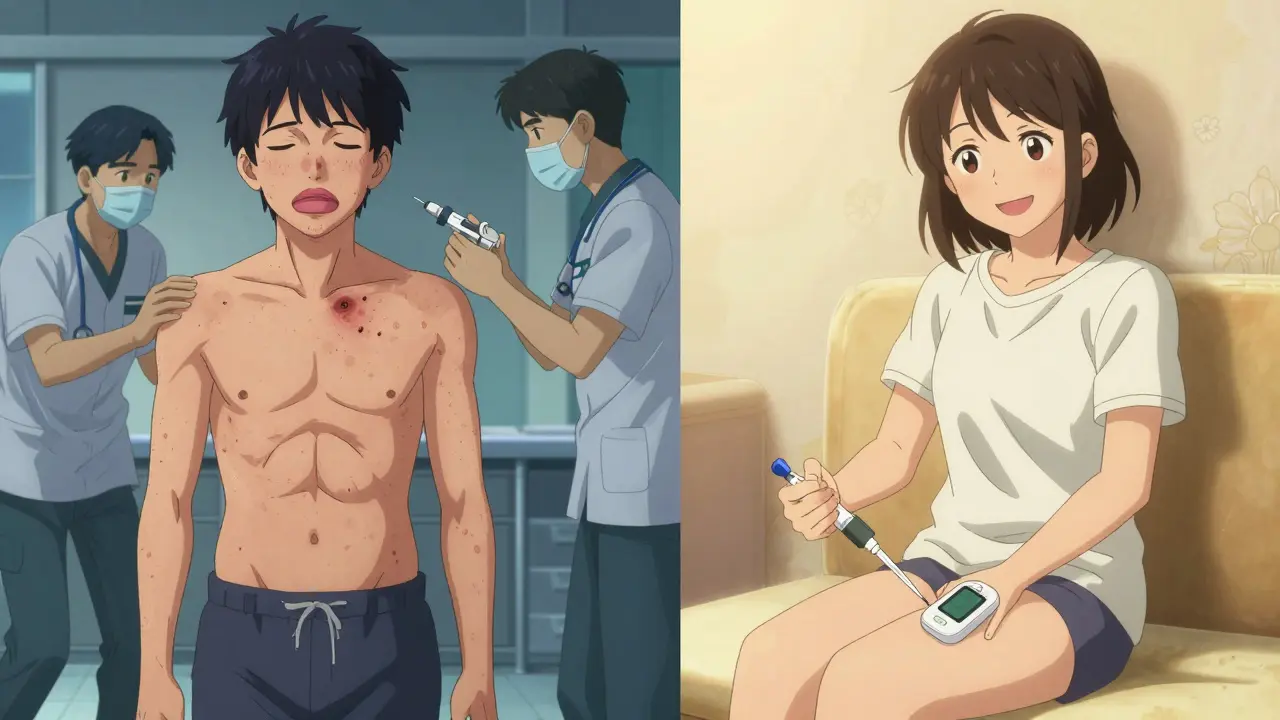
Not all redness or soreness at the injection site means you’re allergic. Common side effects like sweating, shaking, or feeling anxious are signs of low blood sugar, not an allergy. True insulin allergies are immune-driven. They come in three main forms.Localized reactions are the most common. These show up as red, itchy bumps or swelling right where you injected. Sometimes, they turn into hard lumps under the skin that last for days. These usually show up 30 minutes to 6 hours after the shot and fade within 24 to 48 hours in 85% of cases. They’re uncomfortable, but not usually dangerous.
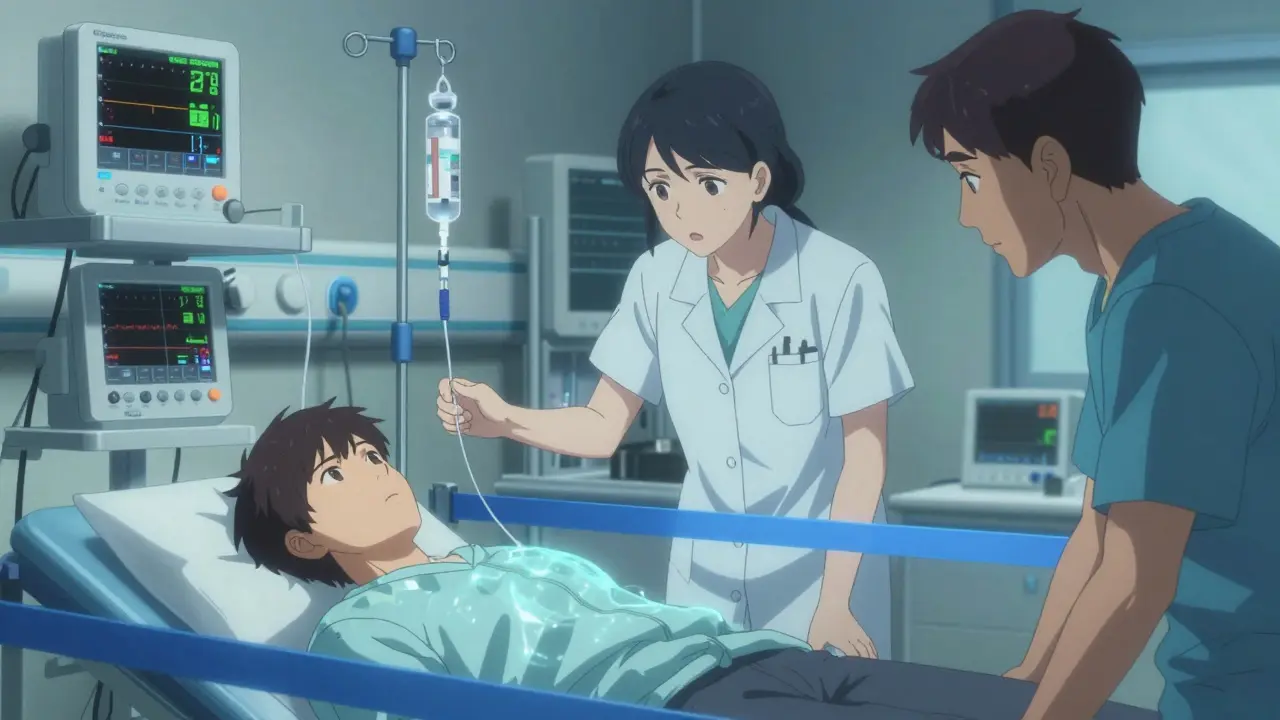
Systemic reactions are rare - under 0.1% of users - but they demand immediate action. Symptoms include hives across the body, swelling of the lips, tongue, or throat, sudden dizziness, trouble breathing, or a drop in blood pressure. These can turn into anaphylaxis, a full-body emergency that can kill within minutes if untreated.
Delayed reactions are the trickiest. You might use the same insulin for years without issue, then suddenly develop joint pain, muscle aches, or deep bruising that takes weeks to fade. These aren’t IgE-mediated like the others. They’re T-cell driven, meaning your body’s immune memory is reacting slowly, not instantly. This type often gets missed because it doesn’t fit the classic allergy profile.
What’s Really Causing the Reaction?
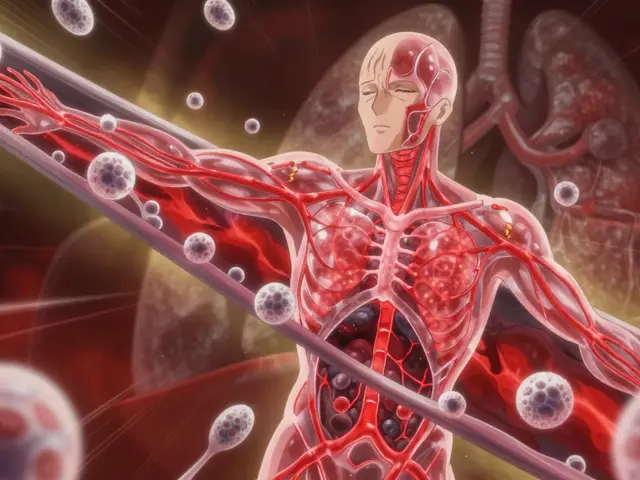
You might think it’s the insulin itself. But in many cases, it’s not. Modern insulins are highly purified, so the protein is less likely to trigger a reaction than the old animal-based versions from the 1930s, which caused allergies in up to 15% of users.More often, the culprit is the excipients - the additives that help insulin stay stable. Two common ones are metacresol and zinc. For example, Humalog contains more metacresol than other insulins. If you’re reacting to one brand and not another, switching could solve the problem without needing complex treatment.
Some people react to the preservatives in the vial or pen, not the insulin molecule. That’s why switching from human insulin to an analog like insulin glargine or insulin lispro can work - even if you’ve had reactions before. About 70% of patients find relief just by changing the type of insulin they use.
How Doctors Diagnose It
If you suspect an allergy, don’t guess. See your diabetes team immediately. They’ll refer you to an allergist for proper testing. The gold standard is skin prick testing or intradermal testing with different insulin types and excipients. Blood tests for specific IgE antibodies can also confirm an IgE-mediated reaction.For delayed reactions, patch testing or biopsy of the affected skin might be needed. These aren’t routine, but they’re essential if symptoms persist after switching insulins or if you’ve had reactions for years without explanation.
Don’t try to self-diagnose. Low blood sugar, infections, or even stress can mimic allergy symptoms. Only a specialist can tell the difference.
What to Do If You React
For mild, localized reactions: Apply a topical calcineurin inhibitor like tacrolimus or pimecrolimus right after injecting. Repeat the application 4-6 hours later. This suppresses the immune response at the skin level without affecting your blood sugar. If that doesn’t help, a mid-to-high potency steroid cream like flunisolide 0.05% applied twice daily for a few days can reduce inflammation and bruising.Antihistamines like cetirizine or loratadine can help with itching and redness. They won’t fix the root cause, but they make daily life manageable while you work on a longer-term solution.
For systemic reactions: Call 999 immediately. Don’t drive yourself. Don’t wait. Anaphylaxis doesn’t wait. If you have an epinephrine auto-injector (like an EpiPen), use it right away. Even if symptoms improve, you still need emergency care - a second wave of reaction can happen hours later.
For delayed reactions: Keep a detailed log. Note the time of injection, the insulin brand and batch, the site, and exactly what happened - swelling, pain, bruising, fever. This helps your doctor spot patterns. You might be reacting to a specific preservative or manufacturing change.
Can You Still Use Insulin?
Yes - and you must. Stopping insulin, even for a few days, can lead to diabetic ketoacidosis (DKA), which is deadly. That’s why the goal isn’t to avoid insulin. It’s to find a way to use it safely.For most people, switching insulin types works. If that fails, desensitization - also called immunotherapy - is the next step. This involves starting with tiny, diluted doses of insulin and slowly increasing them over days or weeks under medical supervision. In one study, 66.7% of patients had their symptoms completely resolved, and another 33.3% saw major improvement.
This isn’t something you do at home. It requires a hospital setting, constant monitoring, and a team that includes both a diabetologist and an allergist. But it works. Patients who complete desensitization can go back to their normal insulin regimen without fear.
In rare cases where neither switching nor desensitization works - and only for type 2 diabetes patients - doctors may consider oral medications like GLP-1 agonists or SGLT2 inhibitors. But for type 1 diabetes, insulin is non-negotiable. There’s no alternative.
What to Avoid
Don’t stop your insulin because you’re scared. That’s the biggest mistake people make. DKA doesn’t care if you’re allergic - it just happens. And once you’re in DKA, you’re in far more danger than you were from the allergy.Don’t assume your reaction is “just irritation.” If it’s new, worsening, or spreading, treat it as serious. Don’t wait for it to get worse before acting.
Don’t use the same injection site repeatedly. Rotating sites reduces skin trauma and helps you spot if a reaction is tied to a specific location or just a specific insulin.
Don’t ignore delayed symptoms. Joint pain or bruising that shows up a day later isn’t “normal.” It’s a signal your immune system is still reacting.
What’s Changing in Treatment
Newer insulin formulations are being designed with fewer immunogenic additives. Some are replacing metacresol with other preservatives that are less likely to trigger reactions. Continuous glucose monitors (CGMs) are making desensitization safer by letting doctors track blood sugar in real time during the process - reducing the risk of hypoglycemia.Researchers are also looking for biomarkers that could predict who’s at risk before they even start insulin. That’s still years away, but it’s the future. Right now, the best tool is awareness - knowing the signs, knowing when to act, and knowing you’re not alone.
Thousands of people live with insulin allergies and still manage their diabetes. They don’t give up. They adapt. They work with specialists. They switch insulins. They go through desensitization. And they keep living.
When to Call for Help
- Call 999 immediately if you have swelling of the throat, tongue, or lips; trouble breathing; dizziness; or sudden skin discoloration.
- Contact your diabetes team within 24 hours if you develop new or worsening redness, swelling, or lumps at injection sites.
- Reach out if you’ve had joint pain or bruising that lasts more than a week after an injection.
- Never stop insulin without talking to your doctor first.
Can you outgrow an insulin allergy?
Insulin allergies don’t typically go away on their own. Unlike childhood food allergies, they’re not usually temporary. But with proper treatment - like switching insulin types or undergoing desensitization - symptoms can disappear completely. Many people who once reacted badly to insulin now use it safely for years.
Is insulin allergy more common with certain types of insulin?
Yes. Older animal insulins caused the most reactions. Today, human insulin analogs like insulin glargine or insulin lispro are much less likely to trigger allergies. However, some brands contain higher levels of preservatives like metacresol - Humalog, for example - which can cause reactions in sensitive individuals. Switching to a different analog often resolves the issue.
Can I use an insulin pump if I’m allergic?
Yes, but only after identifying the cause of your allergy. If the reaction is to a specific insulin, switching to a compatible type for your pump can work. If it’s to preservatives, some pumps allow you to use insulin without certain additives. Always work with your diabetes and allergy team before switching to pump therapy.
Are insulin allergies hereditary?
There’s no clear evidence that insulin allergies are passed down genetically. But people with a history of other allergies - like hay fever, eczema, or food allergies - may be more prone to immune reactions to insulin. It’s not inherited, but your overall immune sensitivity might play a role.
Can I use over-the-counter creams for injection site reactions?
Avoid regular hydrocortisone or anti-itch creams unless your doctor says it’s safe. Some contain ingredients that can irritate sensitive skin or interfere with insulin absorption. For confirmed delayed reactions, topical tacrolimus or pimecrolimus are preferred. Always check with your allergist before using anything on injection sites.
Next Steps if You’re Reacting
1. Write down every reaction: date, time, insulin brand, dose, injection site, symptoms, how long they lasted. 2. Don’t stop insulin. Call your diabetes team today. 3. Ask for a referral to an allergist who’s worked with insulin reactions before. 4. Bring your insulin log and a list of all insulins you’ve used. 5. Be patient - finding the right solution takes time, but it’s possible.You didn’t ask for this. You didn’t choose it. But you’re not powerless. With the right team and the right approach, you can keep using insulin - safely, confidently, and without fear.







Harsh Khandelwal
December 23, 2025 AT 02:03niharika hardikar
December 23, 2025 AT 22:23Aurora Daisy
December 25, 2025 AT 11:36Isaac Bonillo Alcaina
December 26, 2025 AT 18:03Rosemary O'Shea
December 27, 2025 AT 21:43Joe Jeter
December 29, 2025 AT 07:46Sidra Khan
December 30, 2025 AT 12:15Lu Jelonek
December 31, 2025 AT 17:17Ademola Madehin
January 2, 2026 AT 15:29siddharth tiwari
January 3, 2026 AT 02:42suhani mathur
January 3, 2026 AT 02:42Diana Alime
January 3, 2026 AT 19:02Adarsh Dubey
January 4, 2026 AT 02:10Bartholomew Henry Allen
January 6, 2026 AT 02:01