Chronic hepatitis B isn’t just a lab result-it’s a lifelong condition that affects nearly 300 million people worldwide. If you’ve been told you’re HBsAg-positive for more than six months, you’re part of that group. The good news? We now have better tools than ever to manage it. The better news? Most people with chronic hepatitis B can live long, healthy lives-if they know what to do.
What Makes Hepatitis B Chronic?
Most adults who get hepatitis B clear the virus on their own. Their immune system fights it off within six months. But for about 5% of adults-and up to 90% of infants infected at birth-the virus sticks around. That’s chronic hepatitis B. It doesn’t always cause symptoms. Many people feel fine for years. But silently, the virus is attacking the liver, causing inflammation, scarring, and increasing the risk of liver cancer.
The key marker? Hepatitis B surface antigen (HBsAg). If it’s still in your blood after six months, you have chronic infection. That’s the definition used by WHO, AASLD, and EASL. No guesswork. No ambiguity. Just a simple blood test that tells you where you stand.
When Do You Need Treatment?
Treatment isn’t automatic. Not everyone with chronic hepatitis B needs antivirals right away. But guidelines have changed dramatically. In 2024, the World Health Organization made a bold move: recommend treatment for all adults with HBV DNA above 2,000 IU/mL, no matter their ALT levels or liver scarring.
Why? Because waiting for liver damage to show up is too late. By then, the risk of cirrhosis or cancer is already climbing. The old rules-like waiting for ALT to spike or fibrosis to appear-are outdated. Today, the goal is prevention, not reaction.
Here’s how different guidelines break it down:
- WHO 2024: Treat everyone with HBV DNA >2,000 IU/mL, regardless of ALT or fibrosis.
- AASLD 2018 (updated): Treat if HBV DNA >20,000 IU/mL and ALT above normal, or if fibrosis is present-even with lower viral load.
- SABA 2022: Treat HBeAg-positive people over 30 with HBV DNA >2,000 IU/mL, even if ALT is normal.
That’s a lot of numbers. But the trend is clear: treat earlier. Treat more people. Especially if you’re over 30, have a family history of liver cancer, or come from a region where hepatitis B is common-like Asia, Africa, or the Pacific Islands.
What Antivirals Work Best?
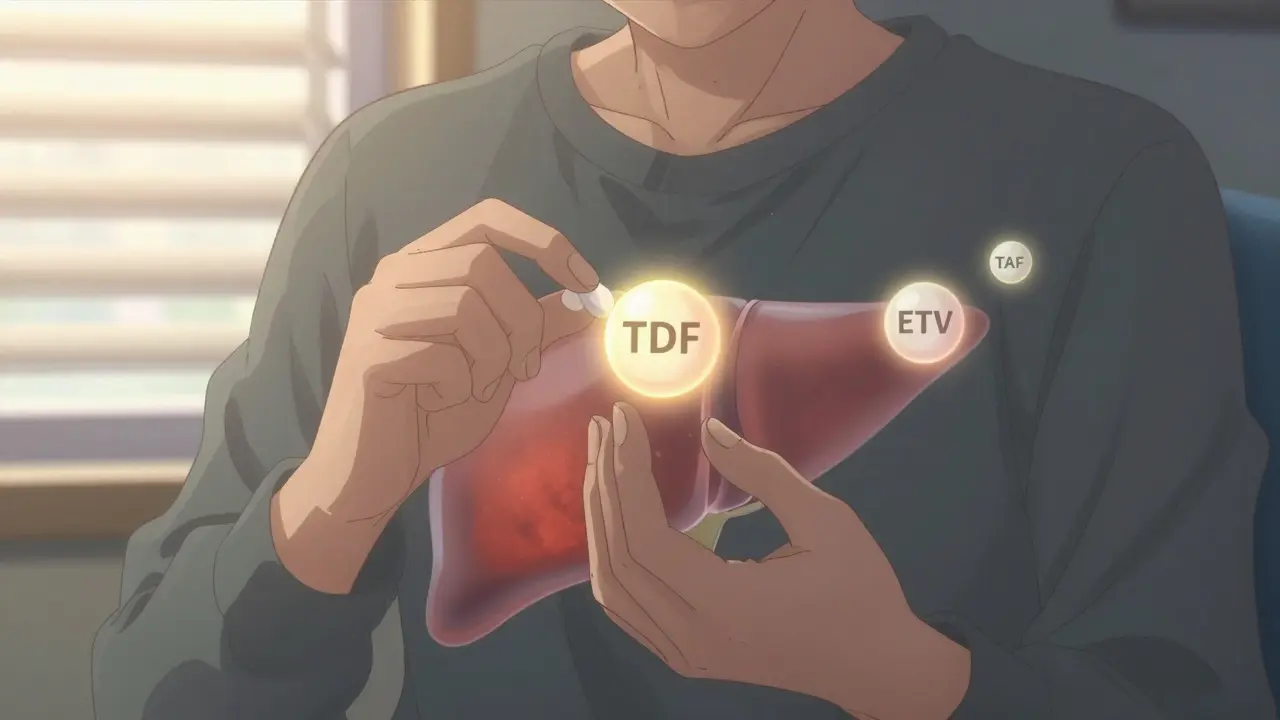
There are three first-line antivirals for chronic hepatitis B: tenofovir disoproxil fumarate (TDF), entecavir (ETV), and tenofovir alafenamide (TAF). All are taken as one pill a day. All are highly effective at suppressing the virus.
But they’re not all the same.
TDF has been around longer. It works great. But it can affect kidneys and bones over time. Studies show it can cause protein in the urine, lower bone density, and rare cases of kidney tubule damage.
TAF, sold as VEMLIDY, is the newer option. It delivers the same antiviral punch as TDF-but at a fraction of the dose. That means less drug in your bloodstream, fewer side effects. Clinical trials show switching from TDF to TAF improves kidney markers and bone density within months.
Entecavir is also safe and effective. It’s often used if you can’t take tenofovir. But it’s not recommended if you’ve had prior lamivudine treatment-resistance can develop.
Pegylated interferon is another option, but it’s rarely used now. It’s given as weekly shots for up to a year. It can cause flu-like symptoms, depression, and fatigue. It’s mostly reserved for younger patients who want a finite treatment course and have a strong immune response.
Bottom line: TAF is now the preferred first-line choice for most people, especially those with kidney issues, osteoporosis, or high blood pressure. It’s not just about killing the virus-it’s about protecting your whole body.
Special Cases: Pregnancy, HIV, and Co-Infections
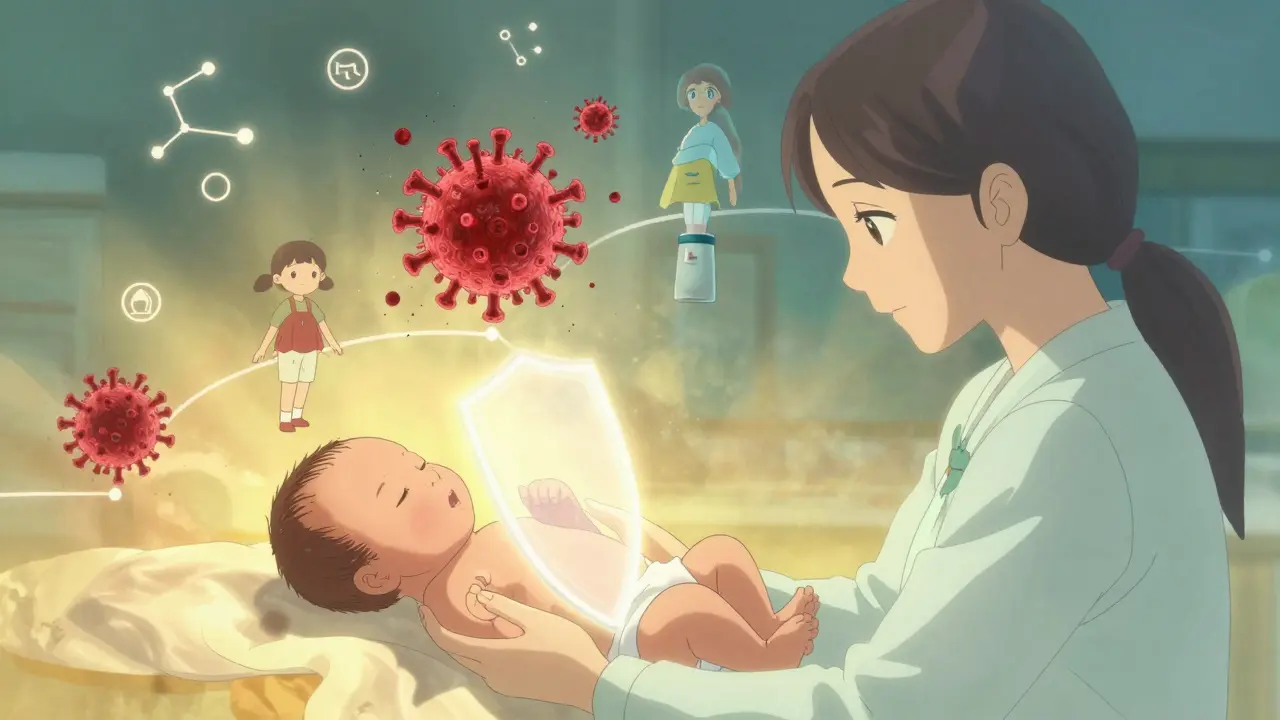
If you’re pregnant and have hepatitis B, your baby is at risk. Without intervention, up to 90% of infants born to HBV-positive mothers become chronically infected. That’s why WHO now recommends tenofovir starting at week 28 of pregnancy for mothers with HBV DNA above 5.3 log10 IU/mL (that’s about 200,000 IU/mL).
It’s simple. Safe. Effective. And it cuts mother-to-child transmission by over 95%.
What if you have HIV too? You don’t need to choose between treatments. All HIV regimens now include drugs that also work against HBV-tenofovir and emtricitabine. You get both viruses treated at once. No extra pills. No extra risk.
And if you’re getting treated for hepatitis C? You still need HBV protection. Even if your HBV is quiet, the hepatitis C cure can wake up the hepatitis B virus. That’s called HBV reactivation. It can cause sudden, severe liver failure. So if you’re HBsAg-positive and starting hepatitis C treatment, you get antivirals too-no exceptions.
Don’t forget hepatitis D. It only infects people who already have HBV. And it’s brutal. It speeds up liver damage. That’s why all HBsAg-positive people should get tested for HDV. It’s not optional. It’s standard care now.
The Vaccine: Your Best Defense
Here’s the thing: hepatitis B is one of the few cancers we can prevent with a vaccine. The hepatitis B vaccine is safe, effective, and given in three shots over six months. It’s been around since the 1980s. It’s part of the newborn shot list in over 180 countries.
If you’re unvaccinated and you’ve had a needlestick injury, unprotected sex with someone who has HBV, or shared needles-you need post-exposure prophylaxis. That means one shot of hepatitis B immune globulin (HBIG) and the first dose of the vaccine, given in different arms, within 24 hours. Do it faster if you can. It’s 85-95% effective at stopping infection.
And if you’ve never been vaccinated? Get started. Now. Even if you’re 50. Even if you think you’re low-risk. Hepatitis B spreads silently. You might not know someone is infected. But your liver doesn’t care about their secrets.
Monitoring: Every Six Months, Not Every Few Years
Chronic hepatitis B isn’t a one-and-done diagnosis. You need ongoing care. Every six months, you should get:
- HBV DNA test
- ALT level
- Hepatitis B surface antigen (HBsAg) and HBeAg status
- Liver ultrasound (to screen for cancer)
- AFP blood test (alpha-fetoprotein, a cancer marker)
Some doctors now also check quantitative HBsAg levels. It’s not yet routine everywhere, but it’s growing. Falling HBsAg levels over time can mean you’re moving toward remission-even if you’re not cured.
And if you’re on antivirals? Don’t stop. Ever. Stopping without medical supervision can cause a dangerous flare-up. The virus can rebound hard. Liver failure can follow. Only stop if your doctor says so-usually after years of suppression and clear signs of immune control.
What’s Next? The Future of Hepatitis B
Right now, antivirals suppress the virus. They don’t cure it. But that’s changing. Scientists are developing drugs that target the virus’s hidden DNA-the cccDNA-that hides inside liver cells and keeps the infection alive. At least 15 of these new drugs are in clinical trials.
Some aim to silence the virus permanently. Others help the immune system recognize and kill infected cells. Early results are promising. Experts predict that by 2030, 30-40% of people with chronic hepatitis B might achieve a functional cure-where the virus is undetectable without drugs, and liver damage stops progressing.
But until then, the tools we have work. The vaccine prevents infection. The antivirals protect your liver. The monitoring catches cancer early. The knowledge is there. What’s missing is action.
If you have hepatitis B, see a liver specialist. Not your GP. Not an urgent care clinic. A specialist who knows the guidelines inside out. They’ll know when to test, when to treat, and when to watch.
If you don’t have it-get vaccinated. It’s one shot, three times. It’s cheaper than a coffee. And it saves lives.
Can you cure chronic hepatitis B?
There is no complete cure yet, but antivirals can suppress the virus long-term, preventing liver damage and cancer. A functional cure-where the virus stays undetectable without treatment-is being researched and may become available for some patients by 2030.
Is hepatitis B contagious through casual contact?
No. You can’t catch hepatitis B from hugging, kissing, sharing food, or using the same toilet. It spreads through blood and body fluids-unprotected sex, shared needles, childbirth, or needlestick injuries. That’s why vaccination and safe practices matter.
Do antivirals have long-term side effects?
Tenofovir disoproxil fumarate (TDF) can affect kidneys and bones over time. Tenofovir alafenamide (TAF) has the same effectiveness with much lower risk. Entecavir is also safe for long-term use. Regular blood tests monitor for any issues.
Can you get hepatitis B even if you’re vaccinated?
Rarely. The vaccine is 95% effective. In very rare cases, people with weakened immune systems might not respond fully. But for healthy people, the vaccine provides lifelong protection. No boosters are needed after the full series.
Why is hepatitis B more dangerous in babies?
Infants’ immune systems don’t recognize hepatitis B as a threat. So 90% of babies infected at birth develop chronic infection. Adults clear it 95% of the time. That’s why vaccinating newborns is critical-it’s the best way to stop the cycle.
Should I get tested for hepatitis B if I’m not at risk?
Yes. Many people don’t know they’re infected because there are no symptoms. If you were born in Asia, Africa, Eastern Europe, or the Pacific Islands, or if you had a blood transfusion before 1992, you should be tested. Even if you think you’re low-risk, testing takes five minutes and can save your life.







Annie Choi
January 14, 2026 AT 15:36Just got my HBsAg results back and I’m not gonna lie-I cried. Not because I’m doomed, but because I finally understand what’s going on. This post? Lifesaver. TAF is now my new BFF. No more kidney panic.
Sarah Mailloux
January 15, 2026 AT 13:28My mom’s from Vietnam and she never got tested. She’s 62 now. I’m dragging her to a hepatologist next week. No more ‘it’s not a big deal’ nonsense. This stuff kills quietly.
Jami Reynolds
January 15, 2026 AT 16:41Let’s be real-Big Pharma pushed TAF because it’s more profitable. TDF works fine. The ‘safer’ narrative is marketing. They don’t want you switching back. Watch the data, not the ads.
Nilesh Khedekar
January 17, 2026 AT 05:21Oh so now we’re treating everyone with >2000 IU/mL? Cool. So when do we start testing every random person at the DMV? Because apparently in the US, ‘low risk’ just means ‘not a drug user or sex worker’.
Amy Ehinger
January 18, 2026 AT 19:21I’ve had HBV since birth. I’m 41. Been on TDF for 8 years. My kidneys are fine, my bones are fine. I get my ultrasounds every six months like clockwork. I’m not cured, but I’m alive. And I’m not scared anymore. This post? Perfect. Just needed someone to say it out loud.
Dan Mack
January 20, 2026 AT 00:12They say ‘vaccine prevents cancer’ but did you know the vaccine was developed using fetal tissue? And the WHO’s new guidelines? All part of the global depopulation agenda. You think they want you healthy? No. They want you dependent.
Crystel Ann
January 21, 2026 AT 22:07My cousin got diagnosed last year. She was terrified. Then she read this and started taking TAF. Now she’s hiking, traveling, even dating again. It’s not the end. It’s just a new chapter. And you’re still the author.
Nicholas Urmaza
January 21, 2026 AT 23:19If you’re over 30 and Asian you should’ve been screened at birth. No excuses. Your doctor didn’t tell you? That’s negligence. Don’t wait for symptoms. By then it’s too late. Get tested. Now.
Niki Van den Bossche
January 22, 2026 AT 13:11Chronic HBV isn’t a disease-it’s a metaphysical condition. The virus is a silent poet, whispering through hepatocytes, rewriting your cellular sonnets. The antivirals? Merely linguistic interventions. The real cure lies in transcending the materialist paradigm of virology. Have you meditated on your HBsAg levels today?
RUTH DE OLIVEIRA ALVES
January 22, 2026 AT 23:47As a medical ethicist, I must emphasize: the WHO’s 2024 guidelines represent a monumental shift toward equity. Millions in low-resource regions now have access to treatment previously deemed ‘non-essential.’ This is public health at its most humane. Thank you for highlighting this.
Frank Geurts
January 24, 2026 AT 03:35Wait-so if you’re HIV-positive and HBV-positive, you’re automatically on tenofovir + emtricitabine? That’s correct. But did you know that in 2023, the CDC reported a 12% increase in HBV reactivation among patients on PrEP? That’s not a side effect-that’s a systemic oversight. You’re being used as a guinea pig.
Amy Vickberg
January 26, 2026 AT 03:21I’m not a doctor but I’ve been reading everything I can. My sister has it. I got tested. Negative. So I got vaccinated. And I’m telling everyone I know. This isn’t just about you-it’s about everyone you love. Don’t wait. Just do it.
Nat Young
January 26, 2026 AT 15:32So the ‘functional cure’ by 2030? That’s a fantasy. The cccDNA is too stable. The immune system is too compromised. They’ve been saying ‘cure is coming’ since 1995. It’s not coming. You’re being sold hope to keep you compliant with lifelong pills.