Every year, over a million people in the U.S. get the wrong medicine because of a simple mistake at the pharmacy. Not because the pharmacist didn’t care. Not because they were sloppy. But because no one checked the label one last time - before walking out the door.
You’ve probably been there. You hand over your prescription. The pharmacist calls your name. You grab the bag, say thanks, and head out. But what if that pill bottle has the wrong dose? Or the wrong name? Or instructions that could hurt you?
The good news? You don’t need to trust the system. You don’t need to hope for the best. You just need to pause for 30 seconds and run a quick, simple check. This isn’t about blaming pharmacies. It’s about being the final safety net - the one that actually works.
Step 1: Confirm Your Name Is Exactly Right
The label must match your full legal name - not a nickname, not a variation, not your spouse’s name. In 2024, nearly 13% of medication errors happened because someone got another person’s prescription. It’s more common than you think. Two patients with similar names - say, Robert Smith and Robin Smith - can easily be mixed up in a busy pharmacy. Check the first, middle, and last name. If it says "Rob Smith" and your ID says "Robert James Smith," that’s a red flag. Ask the pharmacist to double-check. Better safe than sorry.
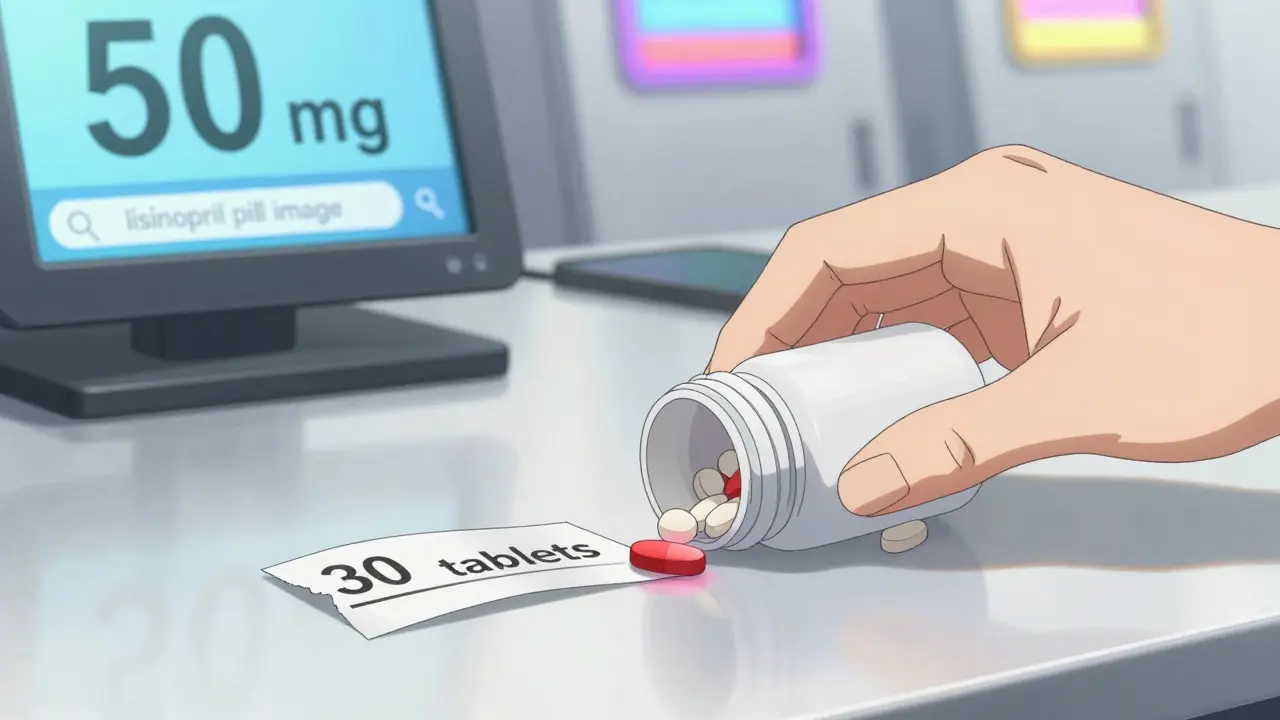
Step 2: Match the Medication Name to Your Prescription
Don’t just read the brand name. Look for the generic name too. Many pills look the same - white, oval, scored - but contain completely different drugs. For example, hydrocodone and hydromorphone sound alike. One treats moderate pain. The other is five times stronger. The FDA recorded over 1,800 cases in 2023 where patients got the wrong drug because of look-alike or sound-alike names. If your doctor prescribed lisinopril, make sure the bottle doesn’t say losartan. Write down the name your doctor gave you. Compare it word-for-word. If you’re unsure, ask: "Is this the same as what my doctor ordered?"
Step 3: Check the Dosage Strength - Numbers and Units Matter
One small mistake can be deadly. 5 mg vs. 50 mg. 10 mL vs. 100 mL. That’s a tenfold difference. In 2024, strength errors were responsible for over a third of serious medication mistakes. Look at the number and the unit together. If the label says "5 mg," make sure your prescription says the same. If it says "take 1 tablet daily," but the bottle says "50 mg tablet," and your doctor only prescribed 5 mg - stop. Don’t take it. Call your doctor or go back to the pharmacy. Don’t assume the pharmacist meant "5 mg" - they wrote "50 mg."
Step 4: Count the Pills or Measure the Liquid
Did your doctor prescribe 30 pills? Does the bottle have 30? Or 60? Or 10? A 2024 CMS audit found that over 8% of errors involved the wrong quantity. Sometimes it’s a counting mistake. Other times, it’s a refill error - you got last month’s prescription again. For liquids, check the volume. If your child’s antibiotic is supposed to be 15 mL per dose and the bottle says 100 mL total, but you were told to take it for 10 days - that’s only enough for 6 doses. Something’s off. Count them. Measure them. Don’t trust the label to be right just because it looks professional.
Step 5: Look at the Expiration Date
Medications don’t just stop working after the expiration date - they can become unsafe. For chronic meds like blood pressure pills or insulin, the FDA recommends they be used within six months of the expiration date. If your bottle says "EXP 03/2025" and today is January 2026, that’s not just expired - it’s past its safe window. Even if it looks fine, don’t take it. Some drugs break down into toxic compounds. Others lose potency and won’t work at all. If the expiration date is too close or already passed, ask for a fresh bottle. Pharmacies are required to give you one.
Step 6: Compare the Pill’s Appearance to What You Expect
Has your pill always been small and white? Now it’s large and blue? That’s not normal. Even if the name and dose are right, the pill’s shape, color, or imprint might be wrong. The FDA’s Drugs@FDA database has pictures of every approved pill. You can search it on your phone. Or ask the pharmacist: "Can you show me what this pill should look like?" Many pharmacies now have printed reference cards or digital screens showing images. If your pill looks different than last time - even if the name matches - speak up. Generic pills change manufacturers often, but the appearance shouldn’t change without warning.
Step 7: Read the Instructions - Out Loud If You Can
"Take one by mouth daily." Sounds simple. But what if it’s supposed to be "take one every 6 hours"? Or "take with food"? Or "do not crush"? A 2023 study found that over 14% of errors came from wrong directions. If the label says "take 2 tablets at bedtime," but your doctor said "take 1 in the morning," you’ve got a problem. Read the instructions slowly. Say them out loud. Then ask yourself: "Does this match what my doctor told me?" If you’re not sure, ask the pharmacist to repeat the instructions. Don’t be shy. It’s their job to make sure you understand.
Why This Works - And Why Most People Skip It
A 2024 study from UCSF showed that when patients follow all seven steps, they catch 87% of errors. That’s nearly nine out of ten mistakes stopped before they reach your body. But only 1 in 3 people actually do it. Why? Because it feels unnecessary. Because you’re in a hurry. Because you trust the pharmacist. And that’s exactly what the system counts on.
But here’s the truth: pharmacists are human. They work under pressure. They fill 200 prescriptions a day. Mistakes happen - even in the best-run pharmacies. The pharmacy’s internal checks are designed to catch errors before the bottle leaves the counter. But they’re not perfect. Your check is the final layer. The last line of defense.

What If You Can’t Read the Label?
Blurry print. Tiny font. Glare from the lights. If you have trouble reading, you’re not alone. Over 60% of adults over 65 struggle with small print on medication labels. That’s not your fault. Pharmacies are required to help. Ask for a magnifying card - most Walgreens and CVS locations now have them. Ask for a large-print label. Ask if they can read the instructions to you. Some pharmacies offer audio labels via QR codes you can scan with your phone. And if you’re caring for someone else - a parent, a partner - do the audit for them. Make it part of your routine.
Tools That Help - But Don’t Replace Your Check
There are apps like MedSafe and FDA MedCheck that scan barcodes and verify prescriptions. They’re great. They catch 98% of errors when used correctly. But they don’t help if you can’t see the screen, if you don’t have a smartphone, or if the barcode is smudged. They also don’t catch things like wrong instructions or mismatched appearance. So use them - but don’t rely on them. Your eyes, your brain, your questions - those are still the most powerful tools you have.
What to Do If You Find a Mistake
If you catch something wrong - don’t panic. Don’t argue. Just say: "I think there might be an error here." Then show them exactly what’s wrong. "The label says 5 mg, but I was prescribed 10 mg." Or "This pill looks different than last time." Most pharmacists will thank you. In fact, pharmacies that encourage patient verification report 73% fewer errors overall. You’re not being difficult. You’re helping them do their job better.
And if they dismiss you? Walk out. Call your doctor. Go to another pharmacy. Your life isn’t worth the convenience of a quick exit.
Make It a Habit
This isn’t a one-time thing. It’s a habit. Do it every single time - even if you’ve taken the same pill for years. Medications change. Prescriptions get updated. New generics come in. What was safe last month might be wrong today. Keep a wallet card with the seven steps. Download a printable version from the CDC’s Medication Safety Kit. Tape it to your bathroom mirror. Set a phone reminder: "Check meds before leaving pharmacy."
Thirty seconds. Seven checks. One life saved.







