Probiotic-Antibiotic Timing Calculator
Why Timing Matters
When you take probiotics at the same time as antibiotics, the antibiotic may kill the probiotic bacteria before they can reach your gut. This calculator helps you determine the optimal time to take probiotics to maximize effectiveness.
Important: Taking probiotics 2-3 hours after your antibiotic dose can reduce your risk of antibiotic-associated diarrhea by up to 50%. This is especially important for preventing C. diff infections.
When you're on antibiotics, you might feel like your body is fighting two battles at once: the infection, and the upset stomach that comes with it. About 1 in 5 people on antibiotics get diarrhea. For some, it’s mild. For others, it’s severe enough to stop the treatment. That’s where probiotics come in-not as a magic fix, but as a tool that can help your gut stay in balance while antibiotics do their job.
Why Antibiotics Mess With Your Gut
Antibiotics don’t pick and choose. They kill the bad bacteria causing your infection-but they also wipe out the good ones living in your gut. Your intestines hold over 100 trillion bacteria, and they’re not just along for the ride. They help digest food, train your immune system, and even make vitamins. When antibiotics disrupt that balance, it can lead to bloating, cramps, and diarrhea. In serious cases, it can trigger Clostridioides difficile (C. diff) infection, a dangerous form of diarrhea that can land you in the hospital.How Probiotics Help
Probiotics are live bacteria and yeasts that are meant to restore what antibiotics destroy. They don’t replace your natural gut flora overnight, but they can give your system a boost while it recovers. The most studied strains for antibiotic-related issues are Lactobacillus rhamnosus GG, Saccharomyces boulardii, and certain Bifidobacterium species. A major 2020 Cochrane review looked at 2454 people taking probiotics alongside antibiotics. The results were clear: those who took probiotics had a 3.1% chance of getting C. diff diarrhea, compared to 11.6% in those who didn’t. That’s more than a 70% reduction in risk. For general antibiotic-associated diarrhea, the benefit was still strong-probiotics cut the odds by nearly half in many cases. Not all probiotics work the same. Saccharomyces boulardii, a yeast, is especially good at surviving stomach acid and antibiotic exposure. One 2018 study showed it reduced diarrhea risk by 50%. L. rhamnosus GG, a bacterial strain, has been shown to reduce side effects by up to 40% in multiple trials. But if you pick a random multi-strain blend from the shelf, there’s no guarantee it’ll help. Quality and strain matter more than the number of billions listed on the label.When and How to Take Them
Timing is everything. If you take your probiotic at the same time as your antibiotic, the antibiotic might kill the probiotic before it can do any good. Most experts recommend spacing them out by at least 2 to 3 hours. Take your antibiotic in the morning and your probiotic at lunch or dinner. That gives the probiotic a window to reach your gut intact. Dosing varies. Most studies use between 5 and 10 billion CFUs (colony-forming units) per day. Some high-dose products go up to 50 billion, but there’s no proof that more is better. Stick to the range of 5-10 billion unless your doctor advises otherwise. Continue taking probiotics for at least one to two weeks after finishing your antibiotic course. Your gut doesn’t recover overnight. Some probiotics work better on an empty stomach, especially those with acid-resistant coatings. Others are designed to be taken with food. Check the label. If it doesn’t say, take it with a light meal to reduce the chance of temporary bloating or gas-common side effects in the first few days.
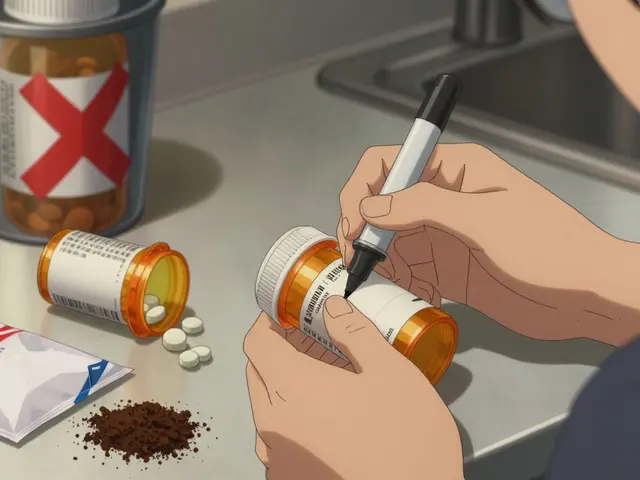
What to Look For (and Avoid)
The probiotic market is a wild west. In the U.S., these products are sold as dietary supplements, not medicines. That means the FDA doesn’t require companies to prove they work or even that they contain what’s on the label. A 2022 ConsumerLab test found that 30% of probiotic supplements didn’t have the number of live organisms claimed. Fifteen percent had extra strains not listed at all. Stick to brands that have been studied in clinical trials. Look for these names on the label:- Lactobacillus rhamnosus GG (Culturelle is a common brand)
- Saccharomyces boulardii (Florastor is a well-known brand)
- Bifidobacterium lactis (found in some yogurts and supplements)
Who Shouldn’t Take Them
For most healthy people, probiotics are safe. But they’re not risk-free. There have been documented cases of people developing serious infections from probiotics-especially those with weakened immune systems. Don’t take probiotics if you:- Have a compromised immune system (from cancer treatment, HIV, organ transplant, etc.)
- Are critically ill or in the ICU
- Have a central IV line or recent surgery
- Have a known yeast allergy (avoid Saccharomyces boulardii)

Real People, Real Results
On Amazon, Culturelle (L. rhamnosus GG) has over 12,500 reviews with a 4.2-star rating. Many users write: “Didn’t get sick while on antibiotics,” or “No more diarrhea after day 2.” But there are also negative reviews: “No effect,” or “Worse bloating than the antibiotics.” Reddit users in r/Probiotics share similar stories. One person took S. boulardii while on a 10-day course of amoxicillin and avoided diarrhea completely. Another, who had IBS, said the probiotic made their cramps worse. That’s why personal experience matters-and why one size doesn’t fit all.The Bigger Picture
Even with strong evidence, not every doctor recommends probiotics. Some say the data isn’t strong enough. Others worry about the lack of regulation. But the consensus among major groups like the International Scientific Association for Probiotics and Prebiotics (ISAPP) is clear: for people on antibiotics, especially those at risk for C. diff, probiotics can be a low-risk, high-reward addition. New research is starting to show something surprising: some probiotics might actually slow down the recovery of your natural gut bacteria after antibiotics. A 2021 study in Nature found that taking certain probiotics delayed microbial balance by months. That’s why experts now say: choose the right strain, use it only during and right after antibiotics, and don’t keep taking it long-term unless you have a reason.Bottom Line
If you’re on antibiotics and worried about stomach issues, probiotics are worth considering. Pick a strain with proven results-L. rhamnosus GG or S. boulardii. Take it 2-3 hours after your antibiotic. Stick with it for two weeks after finishing the course. Don’t overpay for fancy brands. Don’t take them if you’re immunocompromised. And if you’re unsure, ask your doctor. It’s not a cure. It’s a shield. And for many, it makes the difference between getting through antibiotics with a little discomfort-or ending up in the hospital.Can I get probiotics from yogurt instead of supplements?
Yes, but it’s not as reliable. Yogurt contains live cultures, but most commercial brands have low counts and strains that aren’t proven to help with antibiotic side effects. You’d need to eat several servings daily to match the dose in a supplement. For targeted protection during antibiotic treatment, supplements with specific strains like L. rhamnosus GG or S. boulardii are more effective.
How long until I see results from probiotics?
Most people notice a difference within 2-4 days, especially if they’re starting to feel bloated or have loose stools. If you don’t see improvement after 5 days, the strain may not be right for you-or you may need to adjust the timing. Don’t expect miracles, but if diarrhea is prevented or less severe, that’s a win.
Do probiotics interfere with antibiotics?
No, they don’t interfere with how antibiotics fight infection. In fact, some studies suggest they may improve treatment success by keeping your gut healthy enough to tolerate the full course. The key is timing: take them at least 2-3 hours apart to avoid killing the probiotics before they reach your intestines.
Are probiotics safe for kids and elderly people?
For healthy children and older adults, yes-when using the right strains. L. rhamnosus GG is approved for use in children as young as 3 months in some countries. For seniors, especially those on multiple medications, it’s safer to choose a single-strain product and start with a lower dose. Always check with a doctor if the person has chronic illness, a weakened immune system, or a feeding tube.
What if I forget to take my probiotic at the right time?
Don’t panic. If you take it within an hour of your antibiotic, it’s probably fine. If you miss the window by several hours, just take it when you remember. The goal is to avoid taking them together, not to hit a perfect schedule. Consistency matters more than timing precision.
Can probiotics prevent future antibiotic side effects?
Not really. Probiotics help during and right after antibiotic use. They don’t create long-term immunity to side effects. If you take antibiotics again next year, you’ll need to start the probiotic again. There’s no evidence that taking probiotics daily for months builds up lasting protection.






Ali Bradshaw
December 6, 2025 AT 12:19Been on antibiotics twice this year. Took Culturelle both times. First time, zero issues. Second time, I forgot to space them out and ended up with mild cramps. Lesson learned: timing matters more than the brand. Now I take mine at dinner, antibiotic at breakfast. Simple, works.
an mo
December 6, 2025 AT 21:58Probiotics are just corporate snake oil dressed up in lab coats. The FDA doesn't regulate them because they're useless. You think your gut needs a band-aid? It's a microbiome, not a broken pipe. Take the damn antibiotic, suffer through the diarrhea, and let your body heal naturally. No supplements needed. You're not a petri dish.
aditya dixit
December 6, 2025 AT 23:06There’s a quiet wisdom in letting the body restore itself - but also a profound responsibility to use tools that science has validated. L. rhamnosus GG and S. boulardii aren’t magic; they’re ecological buffers. We don’t need to overcomplicate it: when the system is under assault, we don’t abandon the tools that reduce collateral damage. The gut isn’t just digestion - it’s immunity, neurology, metabolism. To ignore evidence because it’s inconvenient is not resilience. It’s ignorance in a hoodie.
Annie Grajewski
December 8, 2025 AT 15:48ok but like… probiotics are just fancy yogurt with a price tag? i took one and my butt was still mad. also why do all these brands say ‘50 billion CFUs’ like that means something? i think they just add glitter and call it science. also i read somewhere that they might make your gut lazy? idk. i’m just here for the memes.
Marvin Gordon
December 9, 2025 AT 02:31My doctor didn’t recommend it, but I did it anyway. Took S. boulardii with my amoxicillin. No diarrhea. No bloating. Just… normal. I’m not some wellness guru - I’m a guy who just didn’t want to spend a week in the bathroom. If you’re on antibiotics and you care about your quality of life, this isn’t optional. It’s basic self-care.
Norene Fulwiler
December 9, 2025 AT 09:32My grandma in Texas takes probiotics every time she’s on antibiotics. She’s 82, doesn’t read labels, swallows two capsules with her coffee. No issues. I asked her why. She said, ‘Honey, if it helps me not cry in the bathroom, it’s worth it.’ Sometimes the science doesn’t need to be complicated to be true.
William Chin
December 9, 2025 AT 22:32It is imperative to note that the consumption of non-pharmaceutical-grade microbial adjuncts may introduce unquantifiable risks, particularly in the context of compromised gastrointestinal integrity. The absence of standardized regulatory oversight renders such interventions ethically dubious and clinically inadvisable absent physician consultation. One must not conflate anecdotal efficacy with evidence-based practice.
Katie Allan
December 10, 2025 AT 03:17I used to think probiotics were a scam until I got C. diff after a round of clindamycin. It took three months to recover. Now I take Saccharomyces boulardii every time I’m prescribed antibiotics - even if I’m just on amoxicillin for a tooth infection. It’s not about being perfect. It’s about not ending up in the hospital because you didn’t want to spend $15 on a pill.
Deborah Jacobs
December 11, 2025 AT 23:18Probiotics are like emotional support bacteria - they don’t fix the problem, but they hold your hand while your gut screams into the void. I took them with my azithromycin and felt like my insides stopped throwing a rave. The first few days? A little gassy. Then boom - peace. No more midnight bathroom marathons. I’m not a scientist. I’m just a person who values sleep and dignity.
Lucy Kavanagh
December 12, 2025 AT 12:36Did you know the FDA allows probiotics to be sold without testing because Big Pharma owns them? They want you to think you need supplements so you keep buying them instead of just eating sauerkraut. Also, the strains listed? Probably not even alive. I read a whistleblower report - they’re just dried dirt in capsules. And the ‘clinical trials’? Funded by the same companies selling it. Wake up.
Chris Brown
December 14, 2025 AT 00:19It is deeply irresponsible to encourage the use of unregulated biological agents in the context of medical treatment. The notion that one can simply ‘pop a pill’ to counteract the necessary destruction of pathogens is not only scientifically naive, but morally reckless. One does not patch a fire with glitter.
Stephanie Fiero
December 14, 2025 AT 03:06ok so i took the probiotic but i took it at the same time as my antibiotic and now i’m gassy AF. like… why does this happen? i thought it was supposed to help?? also i bought the cheapest one on amazon and it didn’t do jack. next time i’m buying the one with the cute bear on it. #probioticfail
Laura Saye
December 15, 2025 AT 03:39It’s fascinating how the gut-brain axis influences not just digestion, but mood regulation and immune modulation. The disruption caused by broad-spectrum antibiotics creates a cascade effect that extends beyond the gastrointestinal tract. Probiotics, particularly S. boulardii, may serve as a homeostatic modulator - not a replacement, but a stabilizer - during periods of dysbiosis. The delay in microbial recolonization observed in the 2021 Nature study suggests that timing and strain specificity are critical variables in restoring ecological balance.
Krishan Patel
December 15, 2025 AT 06:40Probiotics are a scam for people who don’t trust their own bodies. Your gut has been evolving for millions of years. It doesn’t need some corporate lab’s patented bacteria to fix itself. Eat fermented food. Drink water. Rest. Stop buying into the ‘quick fix’ culture. You’re not broken. You’re just sick. Let your body do its job.
Carole Nkosi
December 15, 2025 AT 10:18When I was in Cape Town, my doctor gave me probiotics with my antibiotics. I thought it was weird. But after three days, I felt better than I had in years. Now I tell everyone: if you’re on antibiotics, don’t be stubborn. Take the probiotic. It’s not a luxury. It’s a kindness to your body.