Ever wonder why people with diabetes seem to catch TB more often? The answer isn’t a coincidence - the two conditions interact in ways that make infection more likely and recovery harder. Below we break down the science, the numbers, and what you can do to protect yourself or someone you care about.
What is Diabetes?
Diabetes is a chronic metabolic disorder that impairs the body’s ability to regulate blood glucose. When insulin production or sensitivity is faulty, glucose builds up in the bloodstream, leading to long‑term damage to blood vessels, nerves, and the immune system. Common forms include type1 (autoimmune destruction of insulin‑producing cells) and type2 (insulin resistance often linked to obesity and sedentary lifestyle). In 2023 the International Diabetes Federation estimated 537million adults lived with diabetes worldwide, and that number is still climbing.
What is Tuberculosis?
Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis. It mainly attacks the lungs, but can spread to bones, kidneys, and the brain. People inhale aerosolised droplets from someone with active pulmonary TB; most infections stay dormant (latent TB) and never cause symptoms, yet the bacteria can reactivate when the immune system weakens. The World Health Organization (WHO) reported 10million new TB cases and 1.5million deaths in 2022, making it the leading infectious killer worldwide.
Why Diabetes Raises TB Risk
At first glance, high blood sugar and a lung infection don’t seem related. Dig deeper, and three biological threads emerge:
- Impaired Immune Response: Elevated glucose hampers the function of macrophages and neutrophils, the cells that normally engulf and destroy Mycobacterium tuberculosis. Studies show diabetic patients have 2‑3 times lower production of interferon‑γ, a key cytokine for TB control.
- Chronic Inflammation: Diabetes creates a low‑grade inflammatory state, altering cytokine balance (higher TNF‑α, lower IL‑12). This dysregulation reduces the body’s ability to keep latent TB in check.
- Vascular Damage: Microvascular complications limit oxygen delivery to lung tissue, giving TB bacteria a more hospitable niche.
Combine those factors, and the odds of progressing from latent to active TB jump from about 5% in the general population to roughly 15‑20% in people with uncontrolled diabetes.
Epidemiological Evidence
The link isn’t just theoretical - large‑scale data backs it up. Below is a snapshot of recent findings.
| Study/Region | Diabetes Prevalence Among TB Patients | Relative Risk (RR) of Active TB | Mortality Difference |
|---|---|---|---|
| India, National TB Registry | 15% | 2.5 | +8% (diabetic vs non‑diabetic) |
| South Africa, Cohort Study | 12% | 2.1 | +6% |
| Russia, WHO Surveillance | 18% | 3.0 | +10% |
| Mexico, Urban Hospital | 14% | 2.8 | +7% |
Across continents the pattern holds: diabetes consistently elevates both the risk of catching TB and the chance of a fatal outcome.
Clinical Implications
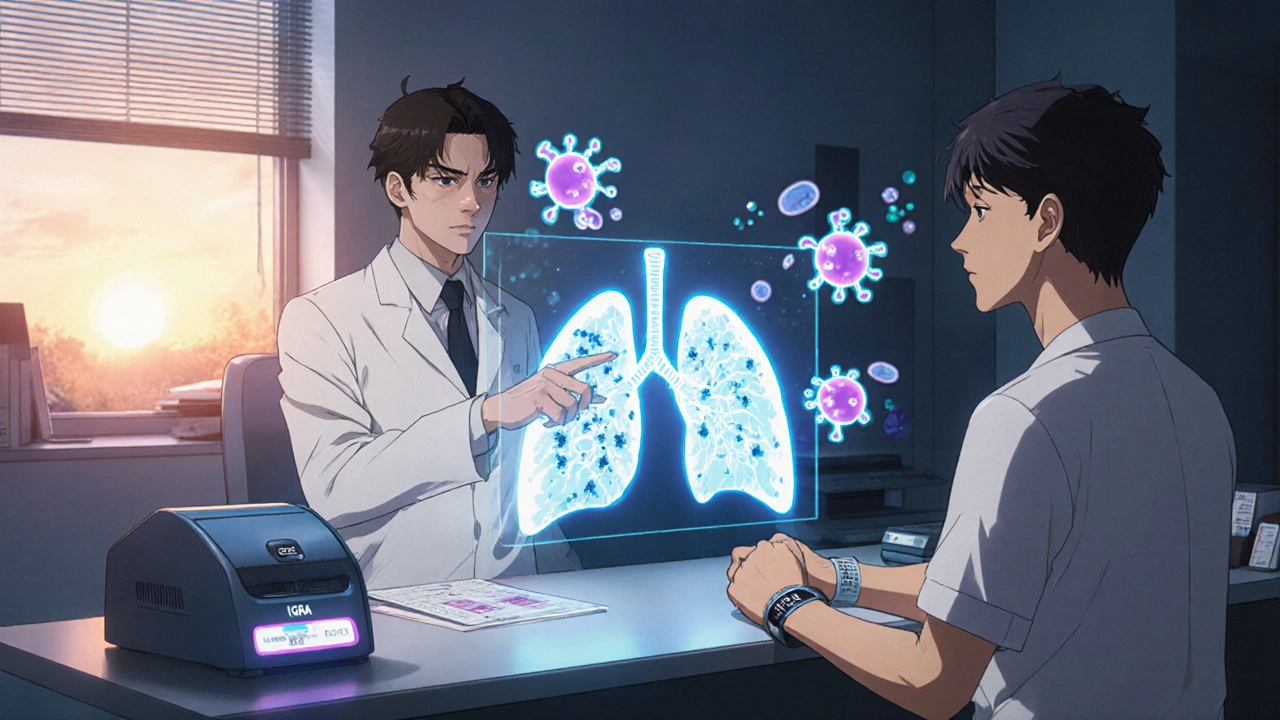
When a diabetic patient presents with a persistent cough, night sweats, or weight loss, clinicians should jump to TB testing sooner rather than later. Here are three practical tips:
- Use both sputum smear microscopy and a rapid molecular test (e.g., GeneXpert) to catch drug‑resistant strains early.
- Screen for latent TB with an interferon‑γ release assay (IGRA) before starting immunosuppressive diabetes meds like steroids.
- Coordinate treatment: Rifampicin can lower blood levels of some oral diabetes drugs, so dose adjustments or switching to insulin may be necessary.
Failure to adjust medications can lead to hyperglycemia spikes, which in turn worsen TB outcomes - a vicious cycle.
Prevention Strategies for People with Diabetes
Preventing TB in diabetic populations isn’t just about antibiotics; it’s a multi‑layered approach:
- Vaccination: The BCG vaccine (BCG vaccine) still offers partial protection against severe TB forms, especially in children. Some countries now recommend a booster for high‑risk adults, including diabetics.
- Regular Screening: Annual chest X‑rays and IGRA tests for diabetics in high‑TB‑burden areas detect latent infection before it awakens.
- Glycemic Control: Keeping HbA1c under 7% cuts the immune‑suppression effect dramatically. A 2021 meta‑analysis found a 30% reduction in active TB risk for well‑controlled diabetics.
- Nutrition & Lifestyle: Adequate protein, vitaminD, and micronutrients bolster immunity; quitting smoking and limiting alcohol also lower TB susceptibility.
- Address Co‑Infections: HIV co‑infection multiplies TB risk. Integrated testing for HIV, diabetes, and TB enables early antiretroviral therapy and antitubercular treatment.

Public‑Health Perspective
Recognising the diabetes and tuberculosis link has reshaped global health policies. In 2023 the World Health Organization issued a joint TB‑diabetes framework that calls for:
- Bidirectional screening: test every TB patient for diabetes and every diabetic for TB.
- Integrated data systems: share laboratory results between TB and diabetes registries.
- Capacity building: train healthcare workers to recognize overlapping symptoms.
- Resource allocation: fund combined outreach programs in endemic regions.
Countries that have adopted these guidelines - such as India, China, and Brazil - report up to a 12% drop in TB mortality among diabetic patients within two years.
Bottom Line
Diabetes&TB are tangled together by immune, inflammatory, and vascular pathways. Ignoring the connection means missed diagnoses, poorer treatment outcomes, and higher death rates. By screening early, controlling blood sugar, and following public‑health recommendations, we can break the cycle.
Frequently Asked Questions
Does having type1 diabetes increase TB risk as much as type2?
Both types raise risk, but type2 is more common in low‑ and middle‑income countries where TB is endemic, so the public‑health impact appears larger. The underlying mechanism-hyperglycemia‑driven immune dysfunction-is similar for both.
Can the BCG vaccine protect adults with diabetes?
BCG’s protection wanes over time, but recent trials suggest a modest benefit (about 15% reduction in severe pulmonary TB) for high‑risk adults, including diabetics, especially when paired with good glycemic control.
How often should a diabetic get screened for latent TB?
In high‑TB‑burden settings, annual IGRA testing is recommended. In low‑burden countries, a one‑time screen at diabetes diagnosis, followed by testing only if symptoms appear, is sufficient.
Does rifampicin affect diabetes medication?
Yes. Rifampicin induces liver enzymes that can lower plasma levels of sulfonylureas and some DPP‑4 inhibitors. Doctors often switch patients to insulin or adjust oral drug doses during TB treatment.
What role does malnutrition play in the diabetes‑TB connection?
Malnutrition weakens immunity further, creating a triple threat: poor nutrition, high blood sugar, and TB bacteria. Addressing protein‑energy deficits and micronutrient gaps is a key part of integrated care programs.






alex montana
October 17, 2025 AT 20:44Wow!!! Diabetes and TB??!! This is crazy... the link is insane!!!
Wyatt Schwindt
October 18, 2025 AT 17:06Good summary
Lyle Mills
October 19, 2025 AT 20:53The immunopathogenesis illustrates a synergistic dysregulation of macrophage phagocytosis and cytokine signaling, exacerbated by hyperglycemic oxidative stress and microvascular insufficiency.
Barbara Grzegorzewska
October 20, 2025 AT 21:53Honestly, this is the epitome of a medical conundrum-definately a case where the science meets the art of healng, and nobody seems to get it right.
Nis Hansen
October 22, 2025 AT 04:26The relationship between diabetes and tuberculosis is more than a statistical coincidence; it is a profound illustration of how metabolic dysfunction can erode immune resilience. When blood glucose levels remain chronically elevated, the very cells tasked with detecting and destroying Mycobacterium tuberculosis are compromised. Macrophages, the first line of cellular defense, lose their ability to produce reactive oxygen species, a key antimicrobial weapon. Neutrophils, too, exhibit reduced chemotaxis, meaning they arrive late to the site of infection. This delay creates a temporal window where the bacilli can establish a foothold. Moreover, the persistent low‑grade inflammation characteristic of diabetes skews cytokine profiles toward a pro‑inflammatory yet ineffective state. Elevated TNF‑α and diminished IL‑12 disrupt the delicate balance required to contain latent bacilli. Vascular damage further limits oxygen diffusion into pulmonary tissue, starving immune cells of the energy needed for a robust response. Clinical data from multiple continents confirm that diabetics have roughly a three‑fold higher risk of progressing from latent to active TB. The mortality gap widens as well, with diabetic TB patients experiencing up to ten percent higher death rates. From a public‑health perspective, this suggests that screening for TB in diabetic clinics is not optional but essential. Conversely, ensuring tight glycemic control can restore, at least partially, immune competence. Lifestyle interventions-diet, exercise, smoking cessation-serve not only to lower HbA1c but also to fortify the host’s defense against inhaled pathogens. In practice, clinicians should adopt a bidirectional screening algorithm, testing every TB patient for diabetes and vice versa. Such integrated care models have already shown measurable reductions in TB mortality in high‑burden nations. Ultimately, recognizing the intertwined nature of these diseases empowers us to break the vicious cycle and improve outcomes for millions.
Fabian Märkl
October 23, 2025 AT 08:13Great insights! 🌟 Managing blood sugar really does give your immune system a fighting chance. Keep spreading the word! 😊
Avril Harrison
October 24, 2025 AT 12:00Interesting read, thanks for sharing.
Natala Storczyk
October 25, 2025 AT 15:46Can you even fathom the horror!!! Diabetes turning our bodies into open doors for TB??? This is a crisis of epic proportions!!!
kendra mukhia
October 26, 2025 AT 18:33Honestly, anyone who dismisses the urgency of this dual epidemic is either willfully ignorant or dangerously complacent.
Bethany Torkelson
October 27, 2025 AT 22:20Listen, the evidence is crystal clear-if you’re not screening diabetics for TB, you’re essentially neglecting a preventable death.
Grace Hada
October 29, 2025 AT 02:06Stop ignoring the data.
nitish sharma
October 30, 2025 AT 05:53Esteemed colleagues, let us unite our efforts to implement integrated screening protocols, thereby safeguarding vulnerable populations through evidence‑based practice.
Rohit Sridhar
October 31, 2025 AT 09:40That’s inspiring! By aligning diabetes management with TB prevention, we can turn statistics around. Together, healthcare providers, patients, and policymakers can create a future where these diseases no longer feed off each other.
Sarah Hanson
November 1, 2025 AT 13:26I appreciate the comprehenive overview, however, some details could be clearer.