More than 90% of prescriptions in the U.S. are for generic drugs. They’re cheaper, FDA-approved, and just as effective. So why do so many doctors still hesitate to prescribe them?
It’s Not About Cost - It’s About Trust
Doctors don’t avoid generics because they don’t care about saving money. Patients do. Health systems do. But many providers still worry - not about price, but about whether the pill in the bottle will work the same way. A 2017 survey of 134 Greek physicians found that nearly 28% didn’t believe generics were therapeutically equivalent to brand-name drugs. Even more concerning: 63% said they needed more detailed data on how generics perform in real-world use before they’d feel comfortable prescribing them more often. That’s not ignorance. It’s caution. And it’s rooted in real experiences. One doctor in a rural clinic told researchers he switched a patient from brand-name levothyroxine to a generic version - and the patient’s TSH levels spiked. He didn’t know it was a rare case of bioequivalence variation in narrow-therapeutic-index drugs. But he did know his patient got worse. So he stopped prescribing generics for thyroid conditions. That’s not irrational. It’s reactive.Who’s Most Skeptical - And Why
Not all doctors feel the same way. The data shows clear patterns. Male physicians, specialists, and those with over 10 years of experience are significantly more likely to doubt generics than their female or younger peers. In the same Greek study, doctors with more than a decade in practice were 40% more likely to say they’d avoid generics for chronic conditions like hypertension or diabetes. Why? Experience doesn’t always mean wisdom. It can mean rigidity. Many of these doctors started their careers when generics were less regulated, when manufacturing quality varied wildly, and when patient complaints about side effects were more common. They remember the bad batches. They remember the lawsuits. And they haven’t seen enough consistent, long-term data to fully let go of those memories. Meanwhile, younger doctors - especially those trained in the last 10 years - are far more open. They’ve been taught that generics meet the same bioequivalence standards as brand names. They’ve seen the FDA’s 80-125% absorption range explained in medical school. But here’s the catch: only 38.7% of U.S. medical schools include structured education on generic drugs in their core curriculum. That means even the ‘open-minded’ ones are often learning on the job.The Knowledge Gap Is Real
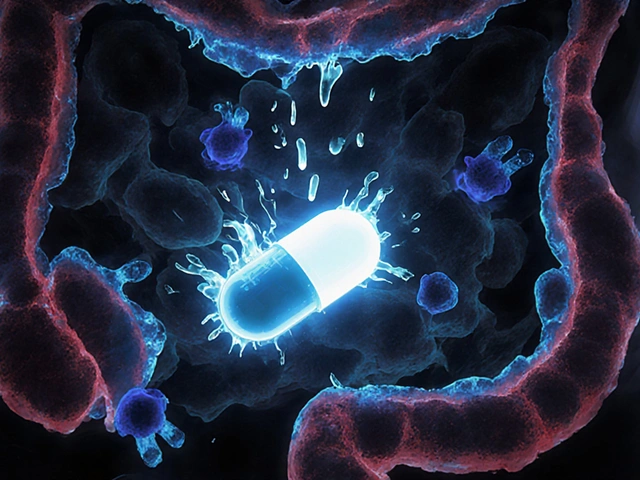
A study from Oxford found that 78% of primary care doctors claimed they were familiar with FDA bioequivalence requirements. But only 44% could correctly define what those numbers actually meant. That’s not a small oversight. It’s a systemic failure. Bioequivalence isn’t about identical absorption. It’s about acceptable variation. A generic drug can be absorbed 20% slower or 25% faster than the brand and still be approved. For most medications, that’s fine. For drugs like warfarin, levothyroxine, or phenytoin - where a 10% shift in blood levels can mean a stroke or seizure - that variation matters. Doctors who understand this nuance are more confident. Those who don’t? They default to what they know: the brand name. And that’s not always about profit. It’s about fear of harm.
What Patients Hear - And What They Believe
Doctors aren’t just prescribing pills. They’re shaping beliefs. When a doctor says, “I’d rather you stay on the brand,” patients hear: “This generic isn’t safe.” Sixty-eight percent of patients learn about generic drugs from their providers. That’s more than from ads, pharmacists, or Google. So when a physician hesitates - even silently - patients pick up on it. They see the brand-name box on the counter. They notice the doctor doesn’t mention the cheaper option. They assume the difference is real. In rural areas, this mistrust has consequences. One CDC study found that 42% of patients stopped taking their medication altogether after being switched to a generic - not because it didn’t work, but because they didn’t trust the switch. And once that trust is broken, it’s hard to rebuild.Education Works - But It Has to Be Right
Here’s the good news: attitudes can change. And they’ve changed before. In Greece, a 90-minute workshop for doctors - focused on real-world data, not regulatory jargon - increased generic prescribing by 22.5% over six months. The biggest jump? Among doctors with 5-10 years of experience. Not the rookies. Not the veterans. The ones in the middle - the ones still learning. The key? Real examples. Not statistics. Stories. Like: “Here’s a patient with high blood pressure who switched from brand to generic. Their BP stayed stable for 18 months. Here’s the lab data.” Peer educators made the biggest difference. Doctors who had successfully switched their own prescribing habits influenced colleagues more than any external speaker. That’s human. That’s real.The Narrow-Index Problem
Some drugs are just trickier. Levothyroxine. Warfarin. Cyclosporine. These are narrow-therapeutic-index drugs. A tiny change in blood concentration can cause big problems. Reddit threads from doctors in r/medicine show this isn’t theoretical. One physician wrote: “I had a patient on warfarin. Switched to generic. INR went from 2.4 to 4.8. No dose change. She almost bled out.” That case wasn’t common. But it was real. And it stuck. The FDA’s 2023 GDUFA III rules now require more post-market data on generics - especially for these high-risk drugs. Early results from Johns Hopkins show that when doctors get access to that data - real patient outcomes, not just lab numbers - their prescribing habits shift. Generic use for newly approved drugs jumped 28.6% in just six months.
Why This Matters Beyond the Prescription
Generics make up 90% of prescriptions in the U.S. But they account for only 23% of drug spending. That’s $528 billion in global savings - if we could just get everyone on board. The problem isn’t the pills. It’s the perception. And perception is shaped by the person handing them out. When a doctor prescribes a generic without hesitation, patients feel safe. When they hesitate, patients feel uncertain. And uncertainty leads to non-adherence. Non-adherence leads to hospital visits. Hospital visits cost money. And lives.What Needs to Change
There’s no single fix. But here’s what works:- Medical schools need mandatory, hands-on training on bioequivalence - not just a slide deck.
- Hospitals and clinics need real-time dashboards showing how generics perform in their own patient populations.
- Pharmacists need to be part of the conversation. They’re more confident in generics than doctors - and patients trust them.
- Regulators need to simplify naming. No more “carbamazepine extended-release.” Try “Carba ER.” Doctors are tired of memorizing chemical names.







Nishant Desae
December 17, 2025 AT 16:13i get why some docs are hesitant, honestly. i had an uncle who switched to a generic thyroid med and his energy dropped off a cliff. he thought it was depression, turned out the generic was absorbing way slower. he went back to brand and boom, back to normal. not every generic is equal, and docs remember these stories. we need better data, not just more pills.
also, why do we still call them 'generics'? sounds like something you buy at a gas station. maybe 'equivalent meds' or something less... cheap-sounding?
Jody Patrick
December 18, 2025 AT 01:02Stop coddling doctors. If it’s FDA-approved, it’s fine. You’re not special. Take the generic and shut up.
Philippa Skiadopoulou
December 18, 2025 AT 12:46The issue is not whether generics work but whether clinicians are equipped to interpret bioequivalence data. The 80-125% range is statistically valid but clinically opaque. Without context, even well-intentioned practitioners default to familiarity. Education must bridge the gap between regulatory science and bedside decision-making.
Pharmacists are often better positioned to explain this. Why aren’t they integrated into prescribing workflows?
Jonathan Morris
December 18, 2025 AT 18:10Let’s be real. The FDA approves generics based on lab tests done on 20 healthy young men in 2003. Meanwhile, real patients have comorbidities, gut issues, liver problems, and take 12 other meds. The system is rigged by pharma to push cheaper pills. The ‘real-world data’ they cite? Mostly funded by generic manufacturers. Wake up.
And don’t tell me ‘it’s 90% of prescriptions’-that’s because insurance forces it. Not because it’s safer. It’s control. Pure and simple.
Anna Giakoumakatou
December 20, 2025 AT 08:38Oh wow. A 90-minute workshop increased prescribing by 22.5%? How revolutionary. Next you’ll tell me that reading a book improves literacy.
Meanwhile, doctors who’ve spent decades seeing patients suffer from inconsistent meds are being told to ‘unlearn’ their lived experience because some statistic says they’re ‘rigid.’ How poetic. The future belongs to the data-literate, and the past belongs to the emotionally compromised.
Also, ‘Carba ER’? Please. That’s not clarity. That’s corporate branding masquerading as medicine.
Martin Spedding
December 21, 2025 AT 05:11One guy’s INR went to 4.8. That’s it. That’s the whole story. That’s why we can’t have nice things.
Also why do we still have 37 different versions of levothyroxine? Who approved this?
Donna Packard
December 22, 2025 AT 02:03I’ve seen this too. My mom switched to generic metformin and got really sick. We went back to brand and she’s fine now. Not everyone reacts the same. I’m not anti-generic-I just want docs to have the freedom to choose what works for each person.
Also, thanks for saying this. I’ve felt weird saying it out loud before.
Patrick A. Ck. Trip
December 23, 2025 AT 17:45It is my considered opinion that the resistance to generic medications stems not from ignorance, but from a deeply rooted ethical imperative to avoid harm.
When a physician prescribes, they are not merely dispensing a compound-they are assuming responsibility for a human life. The bioequivalence thresholds, while statistically sound, do not account for interindividual variability in absorption, metabolism, or adherence.
Therefore, the onus must lie with institutions to provide granular, longitudinal, patient-specific data-not abstract percentages-to support clinical confidence. Without this, we risk conflating cost-efficiency with clinical safety.
Additionally, the suggestion to simplify nomenclature is both pragmatic and humane. The current system is a relic of pharmaceutical marketing, not medical clarity.
Sam Clark
December 24, 2025 AT 18:03One thing I’ve learned in 15 years as a PA: patients don’t care about bioequivalence percentages. They care if they feel better.
When a doctor says, ‘This generic is just as good,’ but looks hesitant, the patient hears, ‘I don’t trust this.’
So we need two things: better education for providers, and better communication training. Not just ‘here’s the data,’ but ‘here’s how to say it so people believe you.’
Also, pharmacists should be on the chart. They know more about this stuff than most docs.
Chris Van Horn
December 25, 2025 AT 22:31Let me guess-this whole article was written by a generic drug lobbyist who got a grant from the NIH and a free trip to a conference in Bali.
Doctors are right to be skeptical. The FDA’s approval process is a joke. You think they test these things on real people? No. They test them on rats. And then they say ‘close enough.’
And now they want to rename drugs? ‘Carba ER’? Are you kidding me? Next they’ll call insulin ‘SugarDown’ and call it a day.
This isn’t progress. It’s corporate control disguised as healthcare reform.
Virginia Seitz
December 26, 2025 AT 10:44My grandma took generic blood pressure med for 5 years. Never missed a beat 😊
Also why is everyone so scared of saving money? 🤔