IBS isn’t just stomach upset. For millions of people, it’s a daily battle with pain, bloating, and unpredictable bowel changes that disrupt work, social life, and sleep. Unlike infections or ulcers, IBS doesn’t show up on scans or blood tests. That’s why it’s often misunderstood - and why so many people suffer for years before getting the right help. If you’ve been told it’s "just stress" or "all in your head," you’re not alone. But here’s the truth: IBS is real, measurable, and manageable - if you know what to look for and where to start.
What IBS Actually Feels Like
People with IBS don’t just have occasional tummy trouble. They experience recurring abdominal pain - often crampy or sharp - that comes and goes over months or years. The pain usually gets worse after eating and improves after a bowel movement. It’s not just about discomfort; it’s about how it changes your life. You might avoid restaurants, cancel plans, or rush home from work because you can’t predict when your body will react.
Along with pain, bloating is one of the most common complaints. The abdomen feels tight, swollen, and visibly distended - even if you haven’t eaten much. Diarrhea can strike suddenly, with urgent, watery stools. Constipation means straining, hard pellets, and that frustrating feeling that you haven’t fully emptied your bowels. Some people switch between both, which is called mixed IBS. Others notice mucus in their stool or feel like they’re constantly gassy.
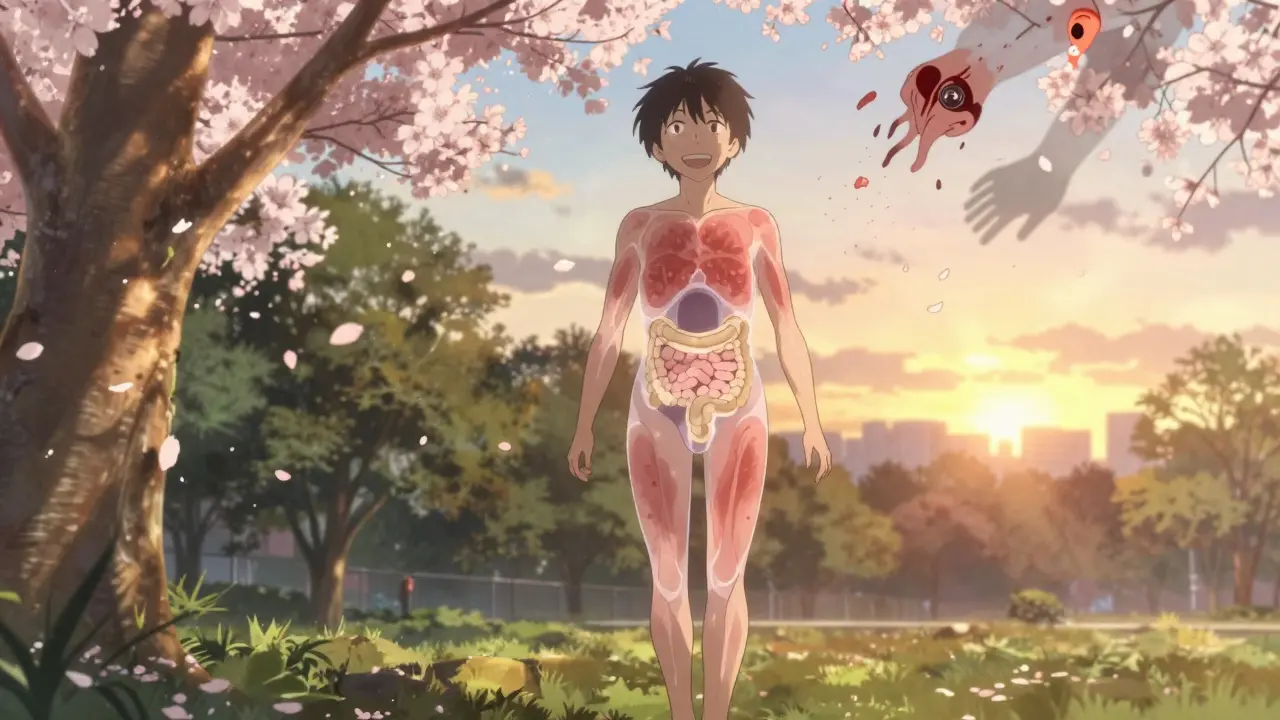
What many don’t realize is that IBS affects more than the gut. About 70% of people with IBS also deal with symptoms like acid reflux, nausea, feeling full too fast, or even chest pain that feels like a heart issue. These aren’t random - they’re part of the same nervous system misfire between your brain and gut.
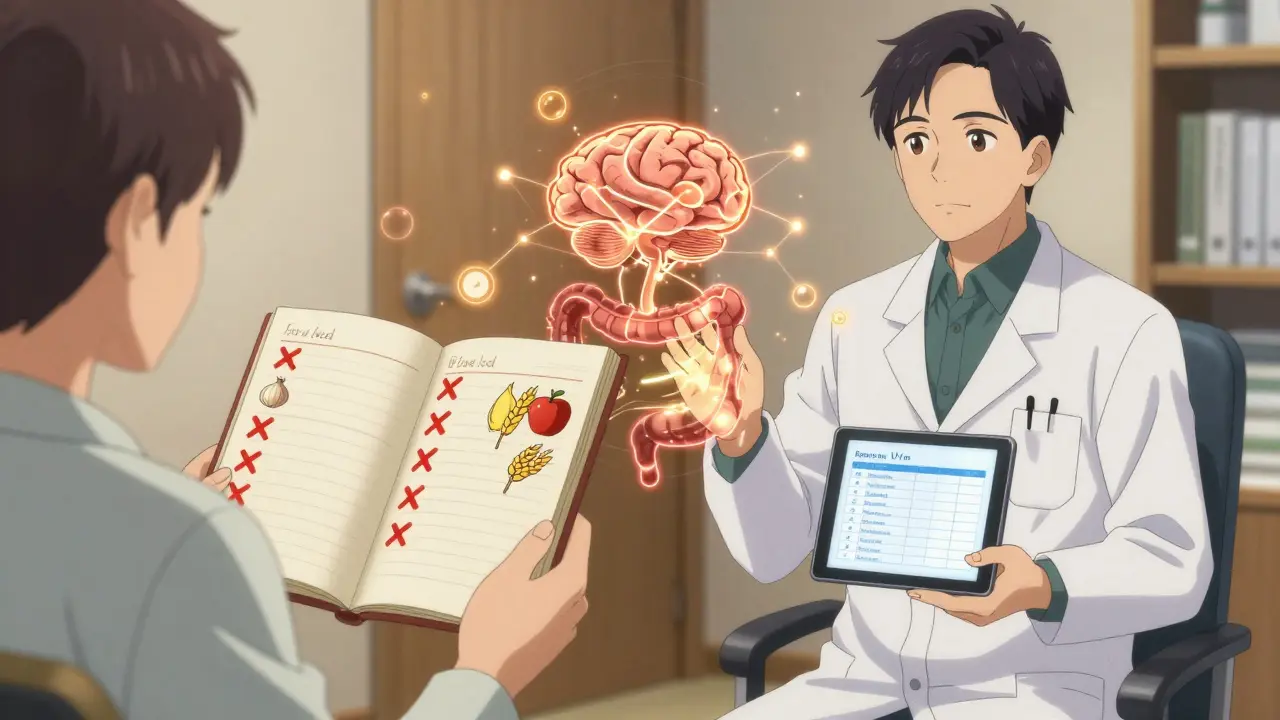
How Doctors Diagnose IBS - And What They Rule Out
There’s no single test for IBS. Diagnosis is based on symptoms that match the Rome IV criteria: abdominal pain at least once a week for three months, linked to bowel movements or changes in stool frequency or form. But before giving that diagnosis, doctors have to rule out other conditions.
Red flags that demand further testing include unexplained weight loss, rectal bleeding, anemia (low iron), or symptoms starting after age 50. Family history of colon cancer or inflammatory bowel disease also raises concern. Blood tests for celiac disease, stool tests for inflammation (like calprotectin), and breath tests for bacterial overgrowth are common. Colonoscopies are usually reserved for older patients or those with warning signs.
Most people get diagnosed after 2-3 doctor visits over 4-8 weeks. That delay is frustrating - and common. On average, people wait over six years from first symptoms to diagnosis. Part of the problem? IBS looks like other things. It mimics food intolerances, thyroid problems, even early-stage colon cancer. That’s why getting the right evaluation matters.
What Makes IBS Flare Up
Triggers vary from person to person, but some patterns are clear. About 70% of people find certain foods make symptoms worse. The biggest culprits? High-FODMAP foods - things like onions, garlic, beans, wheat, apples, milk, and artificial sweeteners. These ferment in the gut, pulling water in and producing gas, which leads to bloating and pain. A low-FODMAP diet, done right with a dietitian, helps 50-75% of people.
Stress is another major trigger. It doesn’t cause IBS, but it turns up the volume. Emotional pressure, anxiety, or even a busy work week can make symptoms flare. Studies show 60-80% of people report worse symptoms during stressful periods. That’s because your gut and brain are wired together - the gut has its own nervous system, called the enteric nervous system, which talks directly to your brain.
For women, hormones play a role. Around 60-70% report worse symptoms just before or during their period. Estrogen and progesterone affect gut motility and sensitivity. Antibiotics can also trigger IBS in about 25% of cases by disrupting the balance of good bacteria in the gut.
Medications That Actually Work
There’s no one-size-fits-all pill for IBS. Treatment depends on your subtype: diarrhea-predominant (IBS-D), constipation-predominant (IBS-C), or mixed (IBS-M).
For IBS-D, two FDA-approved drugs are commonly used: rifaximin (Xifaxan), an antibiotic that targets gut bacteria without affecting the rest of the body, and eluxadoline (Viberzi), which slows bowel movement and reduces pain. About 40-50% of people get relief. Over-the-counter loperamide (Imodium) helps with diarrhea but doesn’t touch the pain or bloating.
For IBS-C, linaclotide (Linzess) and plecanatide (Trulance) increase fluid in the intestines to soften stools. Around 30-40% of users hit the goal of three or more spontaneous bowel movements a week. Lubiprostone (Amitiza) works similarly but is less effective overall. These medications can cause side effects like diarrhea or nausea, especially at first.
Antispasmodics like dicyclomine (Bentyl) or hyoscine (Levsin) have been used since the 1950s. They relax gut muscles and reduce cramping. About 55% of patients report improvement. Low-dose antidepressants - like amitriptyline at 10-30 mg nightly - are surprisingly effective too. Not because you’re depressed, but because they calm the nerves in your gut. About 40-50% of people feel better with these, even if they’ve tried other meds.
Probiotics? Only one strain has solid evidence: Bifidobacterium infantis 35624. It improved symptoms in 35% of people in trials - slightly better than placebo. Most other probiotics don’t help, and some even make things worse.
Beyond Pills: What Really Changes Lives
Medication helps, but it’s not the whole story. The most effective approach combines diet, stress tools, and sometimes therapy.
The low-FODMAP diet isn’t a lifetime sentence. It’s a three-step process: eliminate high-FODMAP foods for 2-6 weeks, then slowly reintroduce them one at a time to find your personal triggers. Most people identify 2-4 specific foods that bother them. Done with a dietitian, this works for 70% of patients.
Cognitive behavioral therapy (CBT) and gut-directed hypnotherapy are backed by strong research. In clinical trials, they reduce symptoms as well as medication - with 40-60% of people seeing big improvements. These therapies help retrain how your brain responds to gut signals, reducing pain perception and anxiety around bowel habits.
Exercise, sleep, and mindfulness practices also matter. Walking 30 minutes a day improves gut motility. Poor sleep worsens pain sensitivity. Even deep breathing exercises can calm the nervous system enough to reduce flare-ups.
What’s Next for IBS Treatment
Research is moving fast. Scientists are studying the gut microbiome in detail and have found distinct bacterial patterns in IBS-D versus IBS-C. A new drug called ibodutant, which targets nerve signals in the gut, showed 45% symptom improvement in early trials - nearly double the placebo rate. Fecal microbiota transplants (FMT), where healthy donor stool is given to restore gut balance, are being tested too. One meta-analysis found 35% of IBS patients went into remission after FMT, compared to 15% in control groups.
But here’s the key takeaway: no matter how advanced the science gets, personalized care still wins. What works for one person might not work for another. That’s why tracking your symptoms - what you ate, how stressed you were, how you slept - is so powerful. Apps or simple journals help you spot patterns your doctor might miss.
Living With IBS - It Gets Better
IBS is chronic, but it’s not life-threatening. Most people learn to manage it well. A 2022 survey of over 1,200 IBS patients found that 62% improved with dietary changes, and 55% felt much better after six months of the right treatment plan. Yes, some days are hard. You might miss work, avoid travel, or feel embarrassed. But you’re not broken. You’re not imagining it. And you’re not alone.
The goal isn’t to be symptom-free every day. It’s to reduce flare-ups enough to live without fear. With the right mix of diet, medication, and mindset, that’s possible - and more common than you think.
Is IBS the same as IBD?
No. IBS (Irritable Bowel Syndrome) is a functional disorder - meaning the gut looks normal but doesn’t work right. IBD (Inflammatory Bowel Disease), which includes Crohn’s disease and ulcerative colitis, involves actual inflammation, ulcers, and damage to the intestinal lining. IBD can be seen on scans and blood tests; IBS cannot. They’re treated very differently.
Can IBS turn into colon cancer?
No. IBS does not increase your risk of colon cancer. But symptoms like weight loss, bleeding, or new-onset changes after age 50 could signal something else. That’s why doctors screen for those red flags - not because IBS turns dangerous, but because other conditions can look like IBS.
Why do I feel bloated even when I eat healthy?
Many healthy foods are high in FODMAPs - things like broccoli, apples, lentils, and yogurt. These can ferment in your gut and cause gas and bloating, even if they’re nutritious. That’s why the low-FODMAP diet isn’t about eating junk - it’s about finding which healthy foods trigger your symptoms. A dietitian can help you keep the good stuff and drop only what hurts.
Do probiotics help with IBS?
Most don’t. Only one specific strain - Bifidobacterium infantis 35624 - has consistent evidence for improving IBS symptoms. Other probiotics may do nothing, or even worsen bloating. If you try one, stick with it for at least four weeks. If you don’t notice a change, stop. Don’t waste money on random brands.
How long does it take for IBS medication to work?
It varies. Antispasmodics and loperamide can help within hours. Linaclotide and rifaximin usually show results in 1-2 weeks. Low-dose antidepressants take longer - 4 to 8 weeks at full dose. Don’t give up too soon. If one drug doesn’t work, talk to your doctor about switching. Finding the right fit often takes trial and error.
Can stress cause IBS?
Stress doesn’t cause IBS, but it makes symptoms much worse. If you already have a sensitive gut, stress activates the brain-gut connection and amplifies pain signals. That’s why therapy, mindfulness, and relaxation techniques are as important as diet and medication. Managing stress isn’t optional - it’s part of treatment.






Chloe Hadland
January 22, 2026 AT 16:35just wanted to say this post made me feel seen. i’ve been told it’s all in my head for years and i cried reading this. you’re not alone, seriously.
Sawyer Vitela
January 23, 2026 AT 22:21low-FODMAP diet doesn’t work for everyone. i tried it for 3 months. zero improvement. also, probiotics are a scam unless you’re buying the one strain they mentioned. everything else is marketing.
Shanta Blank
January 24, 2026 AT 13:53oh sweet jesus i thought i was the only one who had to sprint to the bathroom after eating avocado toast. i used to cancel dates because i’d be in the bathroom for 45 minutes crying. now i carry a change of pants and a bottle of peppermint oil like it’s my job. also, i swear by peppermint tea. it’s witchcraft but it works. 🌿🔥
Kevin Waters
January 25, 2026 AT 20:09the part about low-dose antidepressants was a game-changer for me. i was skeptical too - i’m not depressed, just in constant gut pain. but after 6 weeks on 20mg amitriptyline? my pain dropped by 70%. no magic, just neurology. if you’ve tried everything else, talk to your doc about this. it’s not about mood, it’s about nerve calming.
Sharon Biggins
January 26, 2026 AT 16:31thank you for writing this. i’ve been too scared to say anything out loud because people think i’m exaggerating. i started tracking my food and stress levels in a notebook and it actually helped me find my triggers. not perfect, but better. you’re doing great. 💛
Jamie Hooper
January 28, 2026 AT 15:54so the whole 'stress causes ibs' thing is bs right? i mean, i get that it makes it worse but my doc keeps telling me to 'meditate more' like i'm not already doing yoga, journaling, and breathing exercises like a monk. meanwhile my gut is still screaming. also, why is everyone obsessed with FODMAPs? i eat kale and broccoli daily and still explode. what gives?
Amelia Williams
January 28, 2026 AT 22:50i’m 28 and was diagnosed 2 years ago. i thought i’d be stuck with this forever. but combining low-FODMAP (with a dietitian, not some random blog), daily walks, and gut hypnotherapy? i went from 5 flare-ups a week to maybe one a month. it’s not gone, but i’m living again. if you’re reading this and feeling hopeless - i was there. it gets better. not perfect, but better. and you deserve that.
Himanshu Singh
January 29, 2026 AT 10:21the brain-gut connection is beautiful, really. we think of the gut as just digestion, but it’s a second brain with its own neurons, neurotransmitters, even memories. when stress hits, it doesn't just 'affect' the gut - it speaks directly to it. we’re not broken. we’re wired differently. maybe we need to stop trying to fix the gut and start listening to it. 🌱
Helen Leite
January 30, 2026 AT 06:44they’re hiding the truth. ibs is caused by 5G and glyphosate. the pharma companies don’t want you to know that probiotics are a distraction. i’ve been healing with lemon water and crystals. my symptoms vanished after i stopped eating anything with 'modified starch'. also, my cat purrs on my stomach and it’s 90% cure. 🐱🔮
Husain Atther
January 30, 2026 AT 12:20thank you for the comprehensive overview. i appreciate the distinction between IBS and IBD, as many confuse the two. the evidence-based approach to treatment - especially the emphasis on personalized management - is commendable. for those struggling, patience and consistency are essential. progress may be slow, but it is possible. you are not alone in this journey.