When diabetes damages your kidneys, it doesn’t happen overnight. It creeps in quietly, often without symptoms, until it’s too late. This slow, silent damage is called diabetic nephropathy, and it’s the leading cause of kidney failure worldwide. But here’s the good news: we know exactly how to stop it - if you use the right tools the right way.
What Exactly Is Diabetic Nephropathy?
Diabetic nephropathy starts with tiny leaks in the kidney’s filtering system. These leaks let protein - mostly albumin - escape into your urine. That’s not normal. Healthy kidneys hold onto protein. When you start losing it, your kidneys are under stress. The American Diabetes Association defines it as persistent albuminuria (over 30 mg/g creatinine) on two tests at least three months apart, especially in people with type 1 or type 2 diabetes.
It’s not just about kidney function. Diabetic nephropathy is a warning sign your whole body is struggling. People with this condition are five times more likely to have a heart attack or stroke. That’s why treating it isn’t just about saving your kidneys - it’s about saving your life.
Why Protein Control Matters More Than You Think
Reducing protein in your urine isn’t a side effect - it’s the goal. Every gram of protein leaking out is a sign your kidney filters are being crushed by high pressure. The good news? Lowering that pressure can stop the damage. And that’s where ACE inhibitors and ARBs come in.
These drugs don’t just lower blood pressure. They do something more specific: they relax the tiny blood vessels inside the kidney’s filtering units (glomeruli). This reduces the force pushing protein out. Studies show that when these drugs cut proteinuria by half, the risk of kidney failure drops by up to 70%. That’s not magic. That’s science.
But here’s the catch: you need to take them at maximal tolerated doses. Too many doctors start patients on 10 mg of lisinopril and call it a day. That’s not enough. In clinical trials, the benefits came from doses like 40 mg of lisinopril or 300 mg of losartan - doses that are rarely used in practice because doctors get scared.
ACE Inhibitors vs. ARBs: What’s the Difference?
Both ACE inhibitors and ARBs block the same system - the renin-angiotensin-aldosterone system (RAAS). But they do it in different spots.
- ACE inhibitors (like lisinopril, ramipril, captopril) stop the body from making angiotensin II - the hormone that tightens blood vessels.
- ARBs (like losartan, valsartan, irbesartan) block the receptors that angiotensin II binds to, so even if it’s made, it can’t do damage.
For kidney protection, they’re nearly equal. The RENAAL and IDNT trials proved ARBs reduce kidney failure in type 2 diabetes. The HOPE and MICRO-HOPE trials showed ACE inhibitors do the same in type 1 diabetes. Neither class wins outright. The choice often comes down to side effects.
ACE inhibitors can cause a dry cough in up to 20% of users. ARBs rarely do. If you get a cough on lisinopril, switching to losartan often fixes it - without losing protection.
And here’s something most people don’t know: captopril is the only ACE inhibitor the FDA has officially approved for diabetic nephropathy. But that doesn’t mean others don’t work. Studies show lisinopril and ramipril are just as effective. The approval is historical, not evidence-based.
Dosing Isn’t Guesswork - It’s Science
Guidelines don’t say “take one pill.” They say: titrate to the highest tolerated dose.
Here’s what that looks like in real numbers:
| Medication | Starting Dose | Maximal Tolerated Dose |
|---|---|---|
| Lisinopril (ACEi) | 5-10 mg daily | 40 mg daily |
| Enalapril (ACEi) | 5 mg daily | 20 mg daily |
| Captopril (ACEi) | 25 mg three times daily | 150 mg daily |
| Losartan (ARB) | 50 mg daily | 100 mg daily |
| Irbesartan (ARB) | 150 mg daily | 300 mg daily |
| Ramipril (ACEi) | 2.5 mg daily | 20 mg daily |
These aren’t arbitrary numbers. They’re the doses used in trials that cut kidney failure by half. Yet, studies show only 30-40% of patients ever reach these levels. Why? Fear.
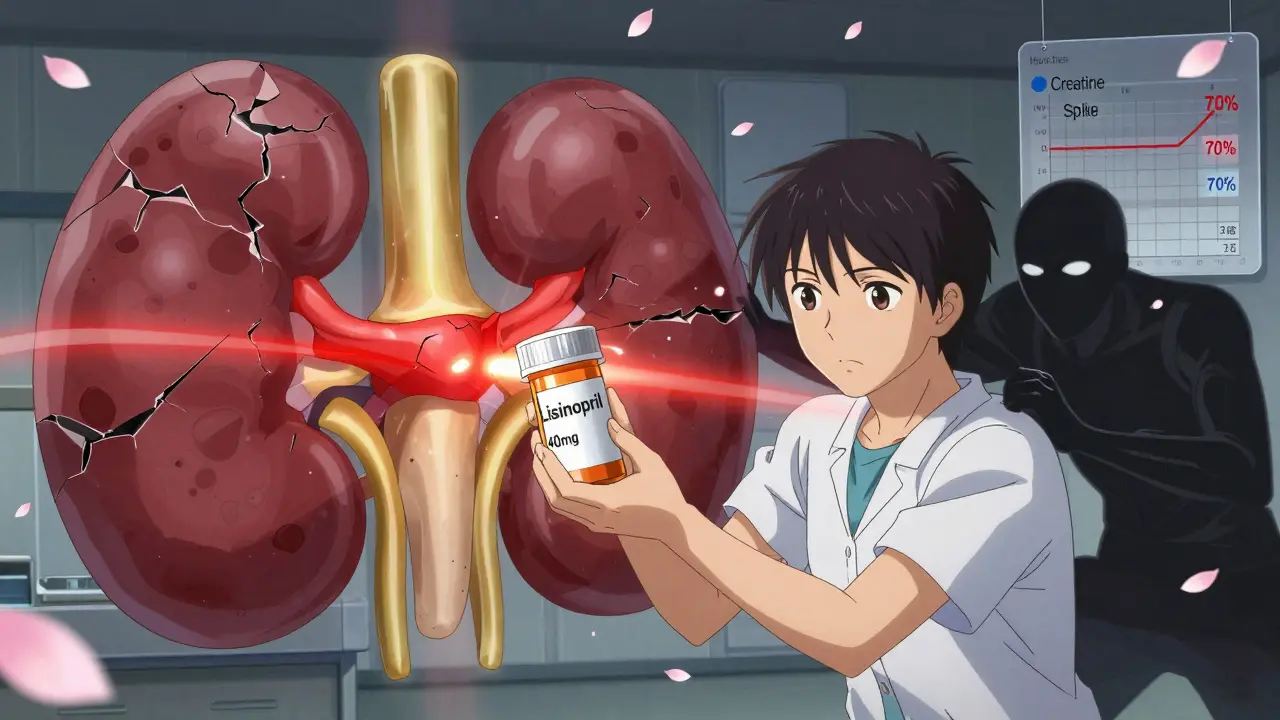
Don’t Stop Because Your Creatinine Rises
This is the biggest mistake in diabetic kidney care.
When you start an ACE inhibitor or ARB, your serum creatinine often goes up - sometimes by 20-30%. Many doctors panic. They stop the drug. They think it’s damaging the kidneys.
It’s not.
A rise under 30% is normal. It means the drugs are working. They’re reducing pressure inside the glomeruli. That pressure was crushing your filters. Lowering it causes a temporary, harmless dip in kidney filtration. It’s like slowing down a car to avoid a crash - the car doesn’t break, it just moves slower.
The American Diabetes Association says this clearly: Do not discontinue these drugs for creatinine increases under 30% unless there’s volume depletion. Stopping them because of this is suboptimal care. It’s like turning off the fire alarm because the smoke detector went off.
Never Combine ACE Inhibitors and ARBs
You might think: “If one is good, two must be better.” Wrong.
The VA NEPHRON-D, ONTARGET, and ALTITUDE trials all tested combining ACE inhibitors with ARBs. Result? No extra kidney protection. Just more danger.
Patients on both drugs had:
- 2-3 times higher risk of hyperkalemia (dangerously high potassium)
- Up to 2 times higher risk of acute kidney injury
- No reduction in death, dialysis, or heart attack
That’s not a combo. It’s a hazard. The National Kidney Foundation warns that adding NSAIDs (like ibuprofen) or loop diuretics (like furosemide) on top of these drugs also spikes kidney injury risk. If you need pain relief, use acetaminophen. If you need fluid control, use thiazides - not loop diuretics - unless absolutely necessary.
What About Newer Drugs Like SGLT2 Inhibitors?
SGLT2 inhibitors (like empagliflozin, dapagliflozin) are exciting. They lower blood sugar, cut heart failure risk, and reduce kidney decline. But here’s the truth: they were tested on top of ACE inhibitors or ARBs.
The EMPA-REG, DAPA-CKD, and CREDENCE trials didn’t replace RAAS blockers - they added to them. That’s why the ADA 2025 guidelines say: “SGLT2 inhibitors should be added to, not substituted for, ACE inhibitors or ARBs.”
If you can’t take an ACE inhibitor or ARB - maybe because of low blood pressure or side effects - then yes, an SGLT2 inhibitor can be your first-line kidney protector. But if you can take them? Start with the RAAS blocker. Then add the SGLT2 inhibitor. Don’t skip the foundation.
Why Are So Many Patients Left Behind?
Studies show only 60-70% of people with diabetic kidney disease get an ACE inhibitor or ARB. Why?
- Doctors don’t know the dosing guidelines
- They fear creatinine spikes
- They don’t realize proteinuria reduction is the goal, not just BP control
- Patients don’t understand why they need to take pills that don’t fix their symptoms
This isn’t a failure of medicine. It’s a failure of implementation. We have the tools. We just don’t use them right.
What Should You Do Now?
If you have diabetes and your urine test shows protein (even just a little), ask your doctor:
- Have I been tested for albuminuria in the last year?
- Am I on an ACE inhibitor or ARB? If not, why not?
- If I am on one, am I at the highest tolerated dose?
- Has my creatinine risen since I started the drug? If so, was it under 30%?
- Am I taking NSAIDs or diuretics that could hurt my kidneys?
If you’re not on one of these drugs and you have high blood pressure or protein in your urine - you need one. If you’re on one but not at the max dose - ask to be titrated up. If your creatinine rose - don’t stop. Ask why.
Diabetic nephropathy doesn’t have to lead to dialysis. It doesn’t have to steal your life. But it won’t stop on its own. You need the right drugs. At the right dose. And you need to stay on them - even when things look scary.
Can ACE inhibitors or ARBs prevent diabetic nephropathy in people with normal kidney function?
No. Studies show that in people with diabetes who have normal blood pressure and no protein in their urine, taking ACE inhibitors or ARBs does not prevent kidney damage. The NIH and ADA guidelines specifically recommend against using these drugs for primary prevention in this group. They’re only recommended once proteinuria or high blood pressure appears.
Is it safe to take an ACE inhibitor or ARB if I have low blood pressure?
It can be, but it needs caution. If your blood pressure is consistently below 110/70 mmHg, your doctor may start at a lower dose or avoid the drug. However, if you have proteinuria, the kidney protection may still outweigh the risk of low BP. Your doctor will monitor you closely. Never stop the drug yourself - talk to your provider first.
Do I need to stop ACE inhibitors or ARBs before surgery?
Sometimes. If you’re having major surgery, especially under general anesthesia, your doctor may ask you to skip your dose the morning of surgery. This is because these drugs can cause a dangerous drop in blood pressure during anesthesia. But you should restart them as soon as you’re stable afterward - usually within 24 hours. Never stop them for more than a day without medical advice.
Can I take an ARB instead of an ACE inhibitor if I have a cough?
Yes. A dry, persistent cough is the most common side effect of ACE inhibitors, affecting up to 20% of users. ARBs don’t cause this. If you develop a cough on lisinopril or ramipril, switching to losartan or valsartan is a safe and effective alternative. You’ll keep the kidney protection without the cough.
What happens if I miss a dose of my ACE inhibitor or ARB?
If you miss one dose, take it as soon as you remember - unless it’s almost time for the next one. Don’t double up. Missing one dose won’t undo the benefits. But regularly missing doses reduces protection. These drugs work best when taken consistently. Set a daily reminder. Your kidneys depend on it.
Final Thought: It’s Not About the Pill - It’s About the Dose
Diabetic nephropathy is preventable. Not with diet alone. Not with sugar control alone. But with the right drug, at the right dose, taken every day. ACE inhibitors and ARBs are not optional. They’re essential. And if your doctor isn’t pushing you to the max tolerated dose - ask why. Your kidneys are listening.