What if you could change how you feel by changing how you think? That’s the core idea behind cognitive-behavioral therapy-or CBT-and it’s not just theory. It’s backed by over 2,000 clinical trials, used by the NHS, recommended by the American Psychological Association, and trusted by millions worldwide.
How CBT Works: Thought Patterns, Not Just Feelings
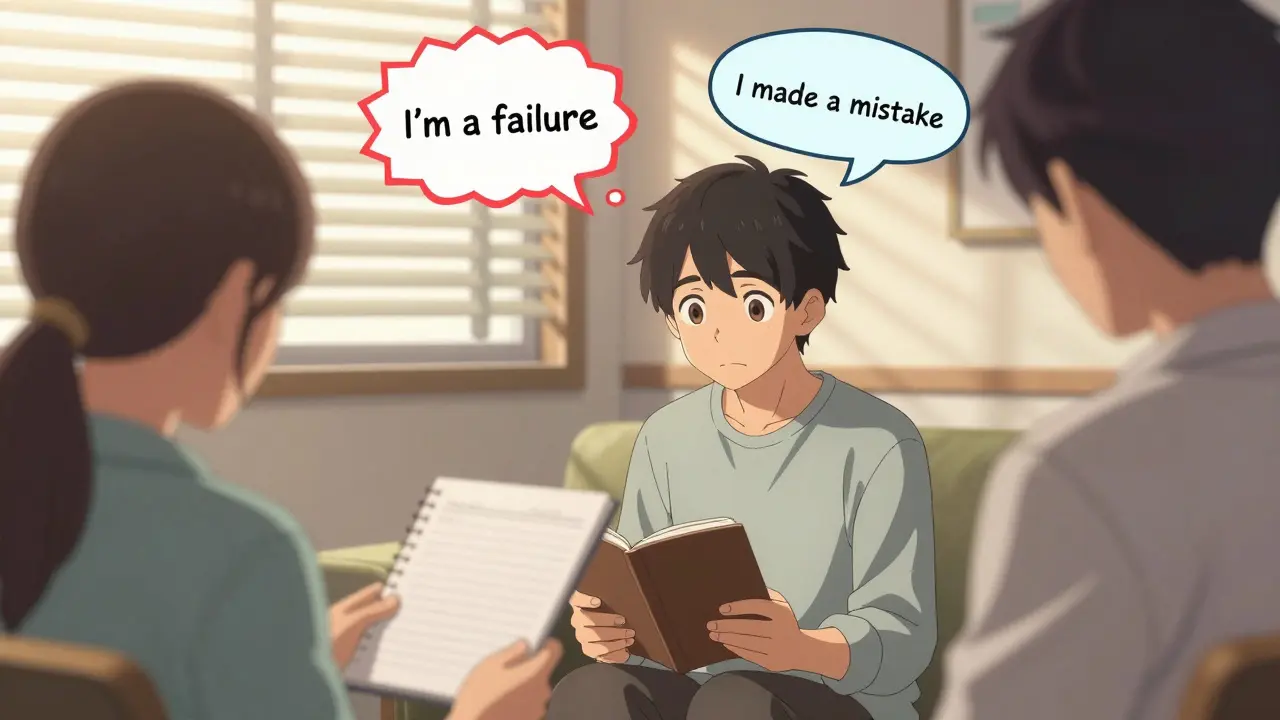
CBT doesn’t focus on your childhood or unconscious drives. It looks at what’s happening right now: the thoughts running through your head when you feel anxious, depressed, or overwhelmed. These thoughts aren’t always true. They’re often distorted. For example, after making a small mistake at work, you might think, “I’m a failure. Everyone thinks I’m incompetent.” That thought triggers shame, a racing heart, and the urge to hide. CBT helps you spot these patterns and test them against reality.The therapy is built on three simple but powerful ideas:
- Distorted thinking contributes to emotional pain.
- Behavioral habits reinforce those feelings.
- You can learn new ways to think and act that reduce suffering.
It’s not about being positive. It’s about being accurate. A person with social anxiety might avoid parties because they believe, “I’ll say something stupid and everyone will laugh.” CBT doesn’t tell them to “just relax.” Instead, they might do a behavioral experiment: attend a small gathering, track what actually happens, and compare it to their prediction. Often, the feared outcome doesn’t occur-or isn’t as bad as imagined.
What Conditions Does CBT Actually Help?
CBT isn’t a one-size-fits-all fix, but it’s been proven effective for a wide range of issues. The National Institute for Health and Care Excellence (NICE) in the UK lists it as a first-line treatment for:- Depression
- Generalized anxiety disorder
- Panic disorder
- Obsessive-compulsive disorder (OCD)
- Post-traumatic stress disorder (PTSD)
- Eating disorders like bulimia
- Chronic insomnia
- Chronic pain
For depression, studies show 60-80% of people see meaningful improvement after 12-16 sessions. In the NIMH’s STAR*D trial, CBT matched antidepressants in effectiveness-but had a much lower relapse rate. After a year, only 24% of those who did CBT relapsed, compared to 52% on medication alone.
For OCD, a specific CBT technique called Exposure and Response Prevention (ERP) is the gold standard. One patient in a 2022 study went from having 15 panic attacks a week to just two after 18 sessions of ERP. For PTSD, CBT helps people process traumatic memories without being overwhelmed by them.
What Happens in a Typical CBT Session?
CBT is structured, time-limited, and practical. Most courses last between 5 and 20 weekly sessions, each about 45-60 minutes long. You’re not just talking-you’re doing.Here’s what you might do in a session:
- Identify a problem: “I can’t go to work because I’m terrified of being judged.”
- Break it down: Using the 5-part model-situation, thought, emotion, behavior, physical sensation-you map out what’s happening.
- Challenge distorted thoughts: “What’s the evidence I’ll be judged? What’s a more balanced thought?”
- Plan a behavioral experiment: “I’ll go to work and notice how many people actually look at me.”
- Do homework: You’ll keep a thought record, practice breathing techniques, or gradually face feared situations.
Homework isn’t optional. It’s where real change happens. A 2021 study found that 45% of people struggle with completing assignments. But those who do are twice as likely to improve. Therapists use motivational techniques to help clients stay on track-not by pushing, but by understanding what’s getting in the way.

CBT vs. Other Therapies: Why It Stands Out
Many people wonder: isn’t talk therapy just venting? CBT is different. Unlike psychodynamic therapy, which can take years, CBT delivers results in weeks. A 2012 meta-analysis of 269 studies found CBT had stronger effects than other therapies for anxiety disorders-effect sizes of 0.77 to 1.14, compared to 0.58 to 0.89 for others.When compared to medication:
- For depression: CBT and antidepressants are equally effective short-term, but CBT lasts longer.
- For substance use: CBT leads to 40-60% abstinence at six months; 12-step programs alone average 25-35%.
But CBT isn’t perfect for everyone. For complex trauma or borderline personality disorder, Dialectical Behavior Therapy (DBT) often works better. For severe childhood behavioral issues, Parent-Child Interaction Therapy has shown 25% better outcomes. And for chronic pain, newer “third-wave” CBT approaches like Acceptance and Commitment Therapy (ACT) can be more effective.
Who Might Not Benefit from CBT?
CBT requires active participation. You need to be able to reflect on your thoughts, do homework, and tolerate discomfort during exposure exercises. That makes it less suitable for:- People with severe cognitive impairment
- Those in acute psychosis
- Individuals who aren’t ready to change
It’s also not a magic fix for deep-seated personality patterns. Critics like Dr. Jonathan Shedler argue it focuses too much on symptoms and not enough on underlying identity. But newer research, including a 2018 meta-analysis, shows CBT can also shift long-term personality traits like self-criticism and emotional avoidance.

Real People, Real Results
Across review sites like Psychology Today and Reddit, 87% of users rate CBT as “very effective” or “extremely effective” for anxiety. One person wrote: “I used to avoid elevators. After six weeks of CBT, I took one-and didn’t panic.” Another said: “The thought record saved me. I wrote down my fears, then I wrote down the facts. The gap was shocking.”But it’s not always easy. About a third of people find homework frustrating. Some feel worse before they feel better-especially during exposure exercises. That’s normal. It’s like physical therapy: it hurts at first, but it builds strength.
How to Find a Qualified CBT Therapist
Not everyone who calls themselves a “CBT therapist” is properly trained. Look for someone who:- Has completed 120-180 hours of formal CBT training
- Has been supervised in at least 20 CBT cases
- Uses structured manuals (like Beck’s or NICE guidelines)
In the UK, the NHS offers CBT through IAPT (Improving Access to Psychological Therapies) services. Private therapists should be registered with the British Association for Behavioural and Cognitive Psychotherapies (BABCP). The Beck Institute trains over 12,000 therapists globally-many of them listed online.
The Future of CBT: AI, Apps, and Personalization
Digital CBT tools like Woebot (FDA-cleared in 2021) have reached over 2 million users. They offer daily check-ins, thought records, and guided exercises. But a 2024 meta-analysis in World Psychiatry found app-based CBT is 22% less effective than in-person therapy-especially for complex cases.The real future lies in precision CBT. Researchers at the National Institute of Mental Health are developing protocols that match treatment techniques to brain activity patterns. Imagine a future where your therapist uses your speech patterns, heart rate variability, and thought records to adjust your treatment in real time.
For now, the best tool is still the human connection-with a trained therapist guiding you through your own mind. CBT doesn’t promise quick fixes. It promises something better: real, lasting change through understanding, practice, and courage.
Is CBT the same as positive thinking?
No. CBT isn’t about forcing yourself to think happy thoughts. It’s about replacing distorted, unhelpful thoughts with more accurate, balanced ones. For example, instead of thinking, “I’ll never get better,” CBT helps you shift to, “I’m having a hard time right now, but I’ve improved before, and I can learn skills to help again.” It’s realistic, not optimistic.
How long does it take to see results from CBT?
Most people start noticing changes within 4-6 weeks. For anxiety or depression, significant improvement often happens by session 8-12. The NHS recommends 12-16 sessions as a standard course. Some people need fewer; others with more complex issues may need 20 or more. Consistency matters more than speed.
Can I do CBT on my own without a therapist?
Yes, but with limits. Self-help books, apps, and online programs (like those from the NHS or Beck Institute) can help with mild to moderate anxiety or depression. But for severe symptoms, trauma, or co-occurring conditions like substance use, working with a trained therapist increases success rates by 40-50%. A therapist helps you spot blind spots, stay motivated, and adjust techniques when they’re not working.
Does CBT work for children and teens?
Absolutely. CBT is one of the most effective treatments for childhood anxiety, OCD, and depression. For younger kids, therapists use games, drawings, and stories to explain concepts. For teens, it’s more like adult CBT but adapted to their language and life stressors. Studies show 63% of adolescents respond well to CBT-slightly lower than adults, but still strong.
Is CBT covered by insurance or the NHS?
In the UK, CBT is freely available through the NHS via IAPT services. In the US, most private insurance plans cover CBT under mental health benefits, especially since CPT codes 90832-90837 are recognized for reimbursement. Twenty-two U.S. states include CBT in their Medicaid programs. Always check your plan’s mental health coverage, but CBT is one of the most widely reimbursed therapies.
What if CBT doesn’t work for me?
It’s not a failure-it’s information. About 20-30% of people don’t respond to CBT, often because the issue is more complex (like trauma or personality patterns) or the fit with the therapist wasn’t right. If CBT doesn’t help, other options include DBT for emotional regulation, EMDR for trauma, or psychodynamic therapy for deeper patterns. The goal isn’t to force one method-it’s to find what works for you.






Oluwatosin Ayodele
December 24, 2025 AT 22:04CBT is just brainwashing with a fancy label. They don't tell you the NHS uses it because it's cheap, not because it's magical. I've seen people do 20 sessions and still end up on disability. The real fix? Get a better job, move out of your parents' basement, and stop scrolling TikTok at 3 AM.
Mussin Machhour
December 25, 2025 AT 17:35Man, I tried CBT last year after my panic attacks got bad. Honestly? It saved me. The thought records were weird at first but after a week I caught myself before spiraling. No magic, just practice. Like lifting weights for your brain.
Rick Kimberly
December 27, 2025 AT 00:54While the empirical support for CBT is indeed robust, one must consider the methodological limitations inherent in many of the cited randomized controlled trials. Publication bias, therapist allegiance effects, and the heterogeneity of diagnostic criteria across studies may inflate perceived efficacy. A meta-analytic review by Hofmann et al. (2012) acknowledges these concerns while still affirming CBT's comparative advantage.
Linda B.
December 27, 2025 AT 19:20Of course CBT works its just what they want you to believe so you dont question the system. The pharmaceutical companies fund half the studies. The NHS pushes it because it costs less than long-term psychoanalysis. They dont want you to dig deeper. They want you to think your thoughts are the problem not your life. Your job. Your rent. Your loneliness. CBT is a bandaid on a severed artery
Christopher King
December 28, 2025 AT 10:22EVERYTHING is CBT now. Therapy? CBT. Parenting? CBT. Your boss giving you feedback? CBT. They turned human suffering into a corporate training module. I used to cry in therapy. Now I fill out worksheets. Where did the soul go? Who decided that our pain could be boxed into a 12-session checklist? I'm not a bug in a system. I'm a human being with a history. And CBT treats me like a glitch to be debugged
Gary Hartung
December 28, 2025 AT 17:51Let me be clear: CBT is not therapy. It is behavioral conditioning. You are not being helped. You are being trained. The goal is not insight, but compliance. The therapist is not a guide. They are a technician. And the patient? A subject. The fact that you call this 'evidence-based' is the most dangerous part. Science is being weaponized to make suffering palatable. You don't need to understand your trauma. You just need to stop thinking about it. And that is not healing. That is suppression.
Ben Harris
December 29, 2025 AT 22:26I did CBT for my anxiety and it worked until I realized my therapist was just reading from a script. I asked about my childhood and she said 'We don't focus on that here.' I paid $180 an hour to be told to breathe and write down thoughts? My dog understands me better. And don't get me started on the apps. Woebot? That's like asking Siri to fix your divorce
Jason Jasper
December 31, 2025 AT 08:02I appreciate the data here. I've seen CBT help people I care about, especially teens. But I also know people who needed something deeper. The article mentions DBT and EMDR - good. Maybe we need to stop acting like one size fits all. Healing isn't a menu. It's a journey. And sometimes you need to sit in the dark before you find the light.
Carlos Narvaez
January 2, 2026 AT 06:57CBT works. Period. If you're not getting results, you're not doing it right. Homework is non-negotiable. If you skip it, you're wasting your time and money. Stop making excuses. This isn't a spa day. It's mental fitness.
Harbans Singh
January 3, 2026 AT 23:15In India, we don't have access to CBT therapists like this. But I've used free apps and books - and it helped. Not perfectly, but enough to get me through. I think the real issue isn't the method. It's access. People need affordable, culturally adapted tools. Not just Western manuals translated into Hindi.
Justin James
January 4, 2026 AT 12:19Did you know the CIA used CBT techniques during Cold War interrogations? They called it 're-education.' The same thought restructuring. The same behavioral exposure. The same homework. They didn't call it therapy. They called it brainwashing. The only difference is who's holding the clipboard. The NHS says it's healing. The military says it's control. Same tool. Different label. Who do you trust? The government? Or your gut feeling that something's off?
Zabihullah Saleh
January 5, 2026 AT 02:49I'm from Afghanistan. We don't have therapists. We have family. We have prayer. We have silence. But when I came here and tried CBT, I was shocked - it felt like someone finally understood how my mind worked. Not by fixing me. But by naming the noise. I didn't need to change my thoughts. I needed to stop fighting them. That's what CBT gave me - permission to be messy.
Winni Victor
January 6, 2026 AT 23:25Oh wow CBT is the new yoga. Everyone's doing it because it's trendy and makes them feel like they're 'working on themselves' while still scrolling Instagram. Meanwhile, their trauma is still buried under a pile of thought records and breathing exercises. At least when you do yoga you get a nice sweat. CBT just gives you a worksheet that says 'You're overthinking it' and charges you $150
Terry Free
January 7, 2026 AT 01:30People who say CBT doesn't work are just weak. You think trauma is solved by crying? No. It's solved by discipline. By doing the work. By showing up. If you can't do homework, you don't deserve to feel better. Stop being a victim. Start being a student.
Lindsay Hensel
January 9, 2026 AT 00:11Thank you for this comprehensive, evidence-based overview. I appreciate the nuanced acknowledgment of CBT’s limitations - particularly its relative ineffectiveness in complex trauma contexts. As a clinician, I have observed that when integrated with attachment-informed practices, CBT becomes not merely a tool, but a bridge. The human connection remains irreplaceable. The structure provides safety; the relationship provides healing.