Antihistamine Safety Checker
Antihistamine Safety Assessment
Risk Assessment
Anticholinergic Score
Select an antihistamine to see its score
Fall Risk
Select an antihistamine to see fall risk comparison
Sedation Risk
Select an antihistamine to see sedation risk
Recommended Alternatives
Key Recommendations
Important: First-generation antihistamines are not safe for older adults. They significantly increase fall risk, confusion, and delirium. If you're taking one of these, talk to your doctor about safer alternatives.
Select an antihistamine to see specific recommendations.
Every year, nearly one in four older adults falls. For many, the cause isn’t just slippery floors or poor lighting-it’s a medication they picked up at the drugstore without thinking twice. First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and brompheniramine are still widely used by older adults for allergies, colds, or even sleep. But these drugs don’t just relieve sneezing-they slow down the brain, blur vision, and throw off balance, turning a simple walk to the bathroom into a life-threatening event.
Why Sedating Antihistamines Are Dangerous for Older Adults
First-generation antihistamines were designed in the 1940s to block histamine, the chemical that triggers allergy symptoms. But unlike modern alternatives, they also cross the blood-brain barrier easily. Once inside, they act like a sedative, depressing the central nervous system. This isn’t just drowsiness-it’s slowed reaction time, poor coordination, and dizziness that lasts for hours. In healthy adults, diphenhydramine clears from the body in about 8.5 hours. In someone over 65, that time stretches to 13.5 hours. The drug lingers, and so do its effects. A 2025 study tracking over 190,000 older adults found that 8% of those who filled a prescription for a first-generation antihistamine fell and needed medical care within 60 days. That’s not a small risk-it’s a pattern. The American Geriatric Society lists these drugs as potentially inappropriate for older adults in their Beers Criteria. Why? Because they don’t just cause falls. They increase the risk of confusion, delirium, constipation, and urinary retention. One study showed older adults on these medications were 2.3 times more likely to develop delirium during a hospital stay-making them even more vulnerable to falling while already weak and disoriented.The Clear Difference Between First- and Second-Generation Antihistamines
Not all antihistamines are created equal. Second-generation options like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were developed to avoid the brain. They stay mostly in the bloodstream, targeting allergy symptoms without the sedation. Here’s what the data shows:- First-generation antihistamines increase the risk of injurious falls by 54% compared to non-users.
- Second-generation antihistamines show no significant increase in fall risk.
- Diphenhydramine has a strong anticholinergic score of 3-4 on the Anticholinergic Cognitive Burden Scale. Fexofenadine? Score of 0.
What You’re Probably Not Realizing: Over-the-Counter Isn’t Safe
Most people think if it’s sold without a prescription, it’s harmless. That’s a dangerous myth. Diphenhydramine is the third most purchased OTC sleep aid in the U.S. for people over 65. Nearly 29 million units were sold last year-mostly to older adults who don’t realize they’re taking a drug linked to falls, fractures, and hospitalizations. Even worse, many don’t know they’re taking it. It’s hidden in multi-symptom cold medicines, nighttime pain relievers, and even some “natural” sleep aids. A pharmacist-led review found older adults typically carry 3.2 high-risk medications in their medicine cabinets-many of them unlabeled or forgotten. The FDA added warnings to OTC labels in 2020, but they’re easy to miss. The labels warn about prostate issues or glaucoma-but rarely mention falls, dizziness, or confusion. That’s a gap. And it’s costing lives.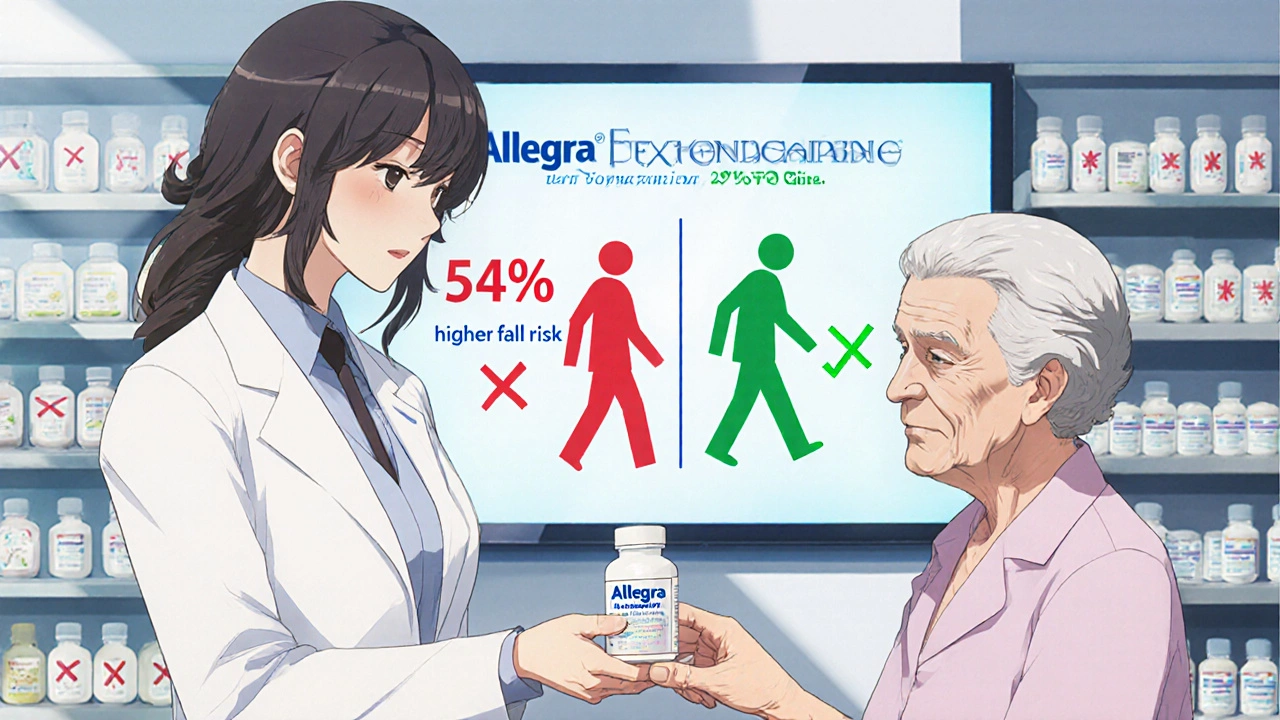
How to Prevent Falls: A Practical 4-Step Plan
Preventing falls isn’t about installing grab bars and buying non-slip mats-though those help. The most powerful step is medication review.- STOP first-generation antihistamines. If you or a loved one is taking diphenhydramine, chlorpheniramine, or brompheniramine, talk to a doctor. Don’t quit cold turkey-especially if used for sleep. But do plan a switch.
- SWITCH to safer alternatives. Fexofenadine is the top choice. Loratadine is a close second. Avoid cetirizine if balance is already an issue.
- REDUCE the dose. If you must use diphenhydramine temporarily, use 12.5 mg instead of 25 mg-and take it at night only. Never take it in the morning.
- REPLACE with non-drug solutions. Nasal saline rinses reduce allergy symptoms by 35-40%. Allergen-proof bedding cuts dust mite exposure by 83%. HEPA air filters remove 99.97% of airborne allergens. These work. And they don’t make you dizzy.
What Healthcare Providers Should Do
Doctors and pharmacists need to be proactive. The CDC’s STEADI initiative recommends a simple three-step approach for every older adult: Stop, Switch, Reduce. During annual wellness visits-now required by Medicare since 2024-providers must screen for fall risk and review all medications. That includes OTC drugs. A 30-minute medication review can uncover hidden dangers. Pharmacists who conduct “brown bag reviews” (where patients bring all their pills in) find an average of 3.2 risky medications per person. In one study, pharmacist-led reviews cut fall rates by 26%. When stopping diphenhydramine for sleep, don’t just cut it. Replace it. Teach sleep hygiene: consistent bedtime, no caffeine after noon, dark and cool room, no screens an hour before bed. These are proven, safe, and effective.
What’s Coming Next: Better Options on the Horizon
The good news? Science is catching up. Two new antihistamines-AGS-2025-01 and FEX-AGE-101-are in Phase II trials. Early results show they cause 89% less drowsiness than diphenhydramine. They’re designed specifically for older adults: minimal brain penetration, no anticholinergic effects, and no lingering sedation. These drugs aren’t on the market yet. But they signal a shift. The old assumption-that one-size-fits-all allergy meds are fine for everyone-is finally being challenged.Final Thought: Your Medication Isn’t Just a Pill
A pill doesn’t just treat an allergy. It changes how you move, think, and react. For an older adult, that’s not a side effect-it’s a hazard. If you’re caring for someone over 65, look at their medicine cabinet. Do you see Benadryl? Chlor-Trimeton? NyQuil? Excedrin PM? These aren’t harmless. They’re silent fall risks. The fix isn’t complicated. Talk to a doctor. Swap the old drug for a new one. Try saline rinses. Improve lighting. Remove rugs. These steps don’t require a prescription. They just require awareness. Because falls aren’t accidents. They’re preventable. And sometimes, the most dangerous thing in the medicine cabinet isn’t the opioid-it’s the antihistamine you bought without thinking twice.Are over-the-counter antihistamines safe for older adults?
No, first-generation over-the-counter antihistamines like diphenhydramine and chlorpheniramine are not safe for older adults. They significantly increase the risk of falls, confusion, and delirium. Even though they’re sold without a prescription, they carry serious risks for people over 65. Safer alternatives like fexofenadine or loratadine are available and should be used instead.
Can I just take a lower dose of Benadryl to stay safe?
Taking a lower dose (like 12.5 mg instead of 25 mg) reduces but doesn’t eliminate the risk. The drug still crosses into the brain and lingers longer in older adults. Even small amounts can cause dizziness and delayed reaction time. The safest approach is to switch to a non-sedating antihistamine like fexofenadine, not just cut the dose.
Why do doctors still prescribe diphenhydramine to older patients?
Many doctors aren’t aware of the updated guidelines, or they assume the patient knows the risks. Others prescribe it because it’s cheap, familiar, or used for sleep. But research shows prescribing patterns haven’t changed much since the 1990s-even though the evidence against it is clear. The American Geriatric Society has warned against it for over a decade, and newer studies confirm the danger.
What are the best non-drug ways to manage allergies in older adults?
Nasal saline irrigation reduces allergy symptoms by 35-40%. Allergen-proof bedding cuts dust mite exposure by 83%. HEPA air filters remove 99.97% of airborne allergens. Keeping windows closed during high pollen seasons and showering before bed also helps. These methods are effective, safe, and don’t carry fall risks.
How do I know if a medication is a first-generation antihistamine?
Look for these active ingredients on the label: diphenhydramine, chlorpheniramine, brompheniramine, doxylamine, or hydroxyzine. These are first-generation. Avoid them. Second-generation antihistamines include loratadine, cetirizine, fexofenadine, and levocetirizine. These are safer for older adults.
Is it safe to use Zyrtec (cetirizine) for older adults?
Cetirizine (Zyrtec) is better than diphenhydramine, but not ideal. It causes drowsiness in about 14% of older adults. Fexofenadine (Allegra) is a safer choice, with only 6% drowsiness. If balance or mobility is already a concern, fexofenadine is the preferred option.






Sean Hwang
November 13, 2025 AT 03:13man i had no idea benadryl was this dangerous for my dad. he takes it every night for sleep and i always thought it was harmless. gonna check his medicine cabinet tonight.
Barry Sanders
November 14, 2025 AT 13:59another ‘woke’ medical article. next they’ll ban aspirin because old people might trip on the bottle cap.
Chris Ashley
November 15, 2025 AT 12:01bro i took diphenhydramine for years and never fell. you’re exaggerating. my grandma takes it and she’s still hiking.
kshitij pandey
November 16, 2025 AT 09:43in india, many elders use antihistamines for colds and sleep too. but we don’t always have access to fexofenadine. maybe we need more affordable safe options? education matters more than just swapping pills.
Brittany C
November 18, 2025 AT 07:38the anticholinergic burden scale is underutilized in primary care. pharmacokinetic changes in geriatric populations necessitate formalized deprescribing protocols, particularly when polypharmacy is present. the data here is robust, yet implementation remains fragmented.
Sean Evans
November 20, 2025 AT 06:13LOL so now we’re blaming benadryl for everything? 🤦♂️ my uncle broke his hip because he tripped over his dog. not because of a pill. people need to stop looking for easy scapegoats. also, why is this even on reddit? 😒
Anjan Patel
November 20, 2025 AT 15:53THIS IS WHY AMERICA IS FALLING APART! PEOPLE TAKE PILLS LIKE CANDY! NO ONE TAKES RESPONSIBILITY ANYMORE! MY GRANDFATHER NEVER TOOK SEDATIVES AND HE LIVED TO 98! YOU’RE ALL WEAK!
Scarlett Walker
November 20, 2025 AT 18:58i switched my mom from benadryl to allegra last year and she’s been so much more alert! no more daytime naps at 2pm. we even started doing yoga together. it’s been life-changing 😊
Hrudananda Rath
November 21, 2025 AT 00:06It is with profound dismay that I observe the proliferation of such rudimentary medical discourse in a public forum. The scientific literature on anticholinergic burden in the geriatric population has been unequivocal since the early 2000s. To reduce this complex pharmacological issue to a Reddit post is not merely reductive-it is an affront to medical epistemology.
Brian Bell
November 22, 2025 AT 03:12my aunt’s pharmacist did a brown bag review and found 5 random pills she didn’t even know she was taking… including a 10-year-old bottle of benadryl. we tossed it all. best decision ever 😎
Nathan Hsu
November 22, 2025 AT 14:15Let me clarify, with precision and due diligence: the data presented, while compelling, does not account for confounding variables such as concurrent use of benzodiazepines, or the prevalence of orthostatic hypotension in this cohort. Therefore, one must exercise caution before drawing definitive causal inferences.
Ashley Durance
November 24, 2025 AT 13:27Actually, the 2025 study you cited has a selection bias-only included patients from urban clinics. Rural elders have different access patterns. Also, cetirizine’s 14% drowsiness rate is still lower than the 30% fall rate from poor lighting. You’re overattributing.
Scott Saleska
November 25, 2025 AT 02:01just to be clear-this isn’t about banning benadryl. it’s about education. i’ve seen so many older people take it because their doctor didn’t explain the risks. maybe we need better labeling or mandatory counseling? just saying.
Ryan Anderson
November 25, 2025 AT 14:08biggest takeaway? if you’re over 65 and taking something with 'PM' in the name, stop. immediately. replace it. your balance will thank you. 🙌