When your heart skips, flutters, or races without warning, it’s not just annoying-it’s dangerous. Atrial fibrillation (AFib) affects more than 33 million people worldwide, and it’s the leading cause of stroke in people over 65. But here’s the thing: not all AFib treatments are the same. Two main strategies exist-rate control and rhythm control-and each comes with different risks, benefits, and best-use cases. And then there’s stroke prevention, which isn’t optional. No matter which path you take, anticoagulation is non-negotiable. So which approach is right for you? Let’s break it down, without the jargon, based on the latest science from 2025.
What Is Rate Control, and When Does It Work?
Rate control means letting your heart stay in AFib but slowing down how fast it beats. The goal isn’t to fix the rhythm-it’s to keep your heart rate under control so your body doesn’t get overwhelmed. Most guidelines say keeping your resting heart rate below 110 beats per minute is enough. You don’t need to hit 70 or 80. The RACE II trial proved that. People who kept their heart rate under 110 did just as well as those who pushed for a stricter target under 80. Fewer side effects. Fewer hospital visits. Same survival rates.
Medications for rate control are simple and well-tested: beta-blockers like metoprolol, calcium channel blockers like diltiazem, and sometimes digoxin. These drugs are cheap, widely available, and usually safe-even for older adults with other health problems. If you’re 75, have diabetes, kidney disease, or high blood pressure, and your AFib doesn’t make you feel terrible, rate control is often the smart first step.
But here’s the catch: rate control doesn’t fix the root problem. Your heart is still in chaos. And if you’re not on a blood thinner, your stroke risk stays high. That’s why anticoagulants like apixaban or rivaroxaban are just as important as the heart rate meds. In fact, the AFFIRM trial showed most strokes happened not because of AFib itself, but because patients stopped their blood thinners or didn’t take them right.
What Is Rhythm Control, and Why Is It Gaining Ground?
Rhythm control tries to restore and keep your heart in its normal, steady beat-sinus rhythm. This used to be reserved for people with terrible symptoms who didn’t respond to rate control. But everything changed after the EAST-AFNET 4 trial in 2020. That study followed nearly 2,800 people with early AFib (average diagnosis under 6 months) for over five years. One group got rhythm control right away. The other got standard care-usually rate control plus anticoagulation.
The results? The early rhythm control group had 21% fewer heart-related deaths, strokes, heart failure hospitalizations, and heart attacks. That’s not a small number. It’s a 3.9% absolute reduction in bad outcomes over five years. That’s like preventing one major event for every 25 people treated early.
How do you do rhythm control? Two ways: drugs or procedures. Antiarrhythmic drugs like flecainide, propafenone, or dronedarone can help, but they’re not perfect. They can cause lung or liver problems, especially amiodarone. That’s why they’re used carefully. The real game-changer is catheter ablation. Ten years ago, complications were common. Today, in expert hands, serious side effects happen in less than 5% of cases. Ablation works best for paroxysmal AFib-when episodes come and go-and for people under 75 with no major heart damage.
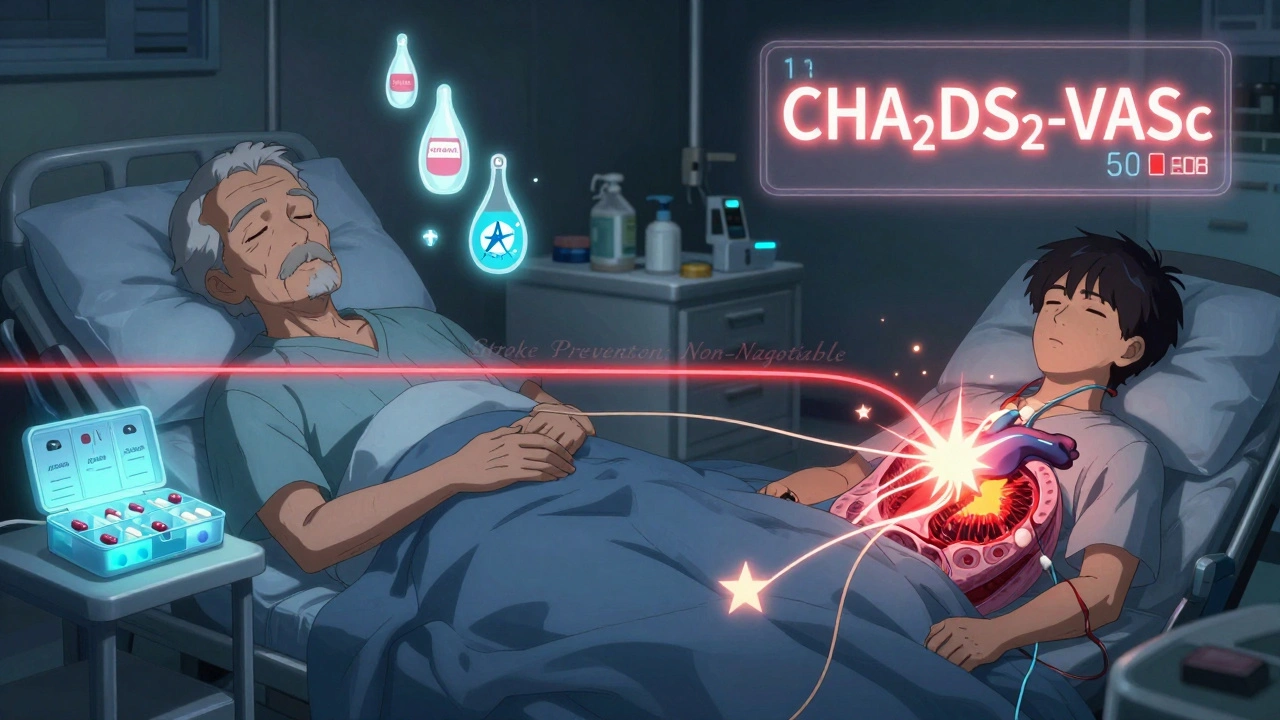
Stroke Prevention: The One Thing You Can’t Skip
No matter if you choose rate control or rhythm control, you still need to prevent stroke. That’s the one rule that never changes. AFib makes your heart’s upper chambers quiver instead of pumping. Blood pools. Clots form. If a clot breaks loose, it can travel to your brain and cause a stroke.
Doctors use the CHA₂DS₂-VASc score to figure out your risk. Points are added for things like age over 75, high blood pressure, diabetes, prior stroke, heart failure, and being female. If your score is 2 or higher, you’re at high risk-and you need a blood thinner. Even if you’re cured of AFib with ablation, you usually still need anticoagulation for at least a few months. Some people need it for life.
Warfarin used to be the only option. Now, direct oral anticoagulants (DOACs) like apixaban, dabigatran, and rivaroxaban are preferred. They’re easier to take, don’t need regular blood tests, and are just as good-or better-at preventing strokes. The key? Don’t miss doses. Even one skipped pill can raise your risk.
Who Should Choose Rate Control?
Rate control isn’t outdated. It’s still the best first choice for many. Think about it this way: if you’re older, have multiple health issues, or your AFib doesn’t bother you much, you don’t need to risk side effects from strong antiarrhythmic drugs or an invasive procedure.
Good candidates for rate control:
- People over 75
- Those with permanent AFib (no plans to restore normal rhythm)
- Patients with severe lung disease, kidney failure, or liver problems
- Those who are asymptomatic or have mild symptoms
- People who can’t access ablation centers or don’t want surgery
The American College of Cardiology says rate control is still appropriate for persistent AFib that’s likely to keep coming back. It’s not about giving up-it’s about choosing the safest, most sustainable path.
Who Should Choose Rhythm Control?
Now, rhythm control isn’t just for the super-symptomatic anymore. The 2023 European Society of Cardiology guidelines say: offer early rhythm control to all patients with AFib, regardless of symptoms. That’s huge. It means if you’re diagnosed with AFib and you’re under 75, you should at least talk about rhythm control-even if you feel fine.
Best candidates for rhythm control:
- People under 65
- Those with paroxysmal AFib (episodes that start and stop)
- Patients with heart failure, even if their ejection fraction is normal
- Anyone with a CHA₂DS₂-VASc score of 2 or higher
- People whose quality of life suffers from AFib-fatigue, shortness of breath, dizziness
Studies like EAST-AFNET 4 show that early rhythm control doesn’t just reduce symptoms. It reduces death and hospitalization. If you’re young and active, and you’ve just been diagnosed, getting rhythm control early might mean you avoid years of heart strain, fatigue, and the slow decline that AFib can cause.
The Real Difference: Symptom Relief vs. Long-Term Survival
Here’s what most people don’t realize: rate control and rhythm control aren’t just about heart rate. They’re about your life.
Rate control keeps your heart from racing, but you’re still living with AFib. You might feel tired, winded, or just ‘off.’ You might need to cut back on activities. You might worry every time your heart skips.
Rhythm control, especially with ablation, can give you back your normal life. People who’ve had successful ablation often say they feel like they did 10 years ago-no more sudden palpitations, no more anxiety about exercise, no more wondering if they’re having a stroke.
But it’s not magic. Ablation isn’t always a one-time fix. About 20-30% of people need a second procedure. It takes time to recover. You still need anticoagulants for months after. But for the right person, the payoff is huge.
What’s Changing in 2025?
The old idea-that rate control is safer and just as good-is fading. New data shows rhythm control, especially early, saves lives. Ablation techniques are better, safer, and more accessible. New drugs like vernakalant and others are in trials, with fewer side effects.
But access is still uneven. In the UK, Europe, and parts of Canada, early rhythm control is becoming standard. In the US, many doctors still default to rate control out of habit. If you’re diagnosed with AFib, don’t accept the first answer. Ask: Is early rhythm control right for me? Ask about ablation. Ask about DOACs. Ask about follow-up plans.
The future of AFib isn’t just managing it. It’s beating it-early, safely, and for good. And that’s a goal worth fighting for.
What About Lifestyle?
Medications and procedures matter-but so do your habits. Weight loss, cutting alcohol, treating sleep apnea, and managing stress can reduce AFib episodes by up to 60%. One study found that losing just 10% of body weight doubled the chance of staying in rhythm after ablation. That’s not a side note. It’s part of the treatment.
If you’re overweight, have high blood pressure, or drink more than one drink a day, fixing those things isn’t optional. It’s part of your rhythm control plan.
Is rate control safer than rhythm control?
Rate control is generally safer in the short term because it uses simpler medications with fewer side effects. But rhythm control, especially with modern ablation, has become much safer than it was 15 years ago. The bigger question isn’t safety-it’s long-term outcomes. Rhythm control reduces death, stroke, and hospitalization over time, especially when started early. So while rate control may seem safer at first, rhythm control can be safer for your future.
Do I still need blood thinners if I get my heart back in rhythm?
Yes, you do-at least for a while. Even after successful ablation or cardioversion, your heart needs time to heal. Blood clots can still form in the first few months. Guidelines recommend continuing anticoagulants for at least 2-4 weeks after rhythm restoration. For people with a high stroke risk (CHA₂DS₂-VASc score ≥2), long-term anticoagulation is often needed permanently, regardless of rhythm.
Can I switch from rate control to rhythm control later?
Absolutely. Many people start with rate control because it’s simpler, then switch to rhythm control if symptoms get worse or if they want to improve their quality of life. There’s no rule that says you have to pick one forever. If you’re still feeling fatigued or limited after months on rate control, talk to your doctor about ablation or antiarrhythmic drugs. It’s never too late to try for better outcomes.
Is ablation worth the risk?
For the right person, yes. Complication rates for ablation have dropped below 5% in major centers. Serious risks like stroke or heart damage are rare. The benefit? For people under 75 with paroxysmal AFib, ablation can restore normal rhythm in 70-80% of cases after one or two procedures. That means fewer medications, less fatigue, and lower long-term stroke risk. If your symptoms are affecting your life, the risk-reward ratio favors ablation.
What’s the biggest mistake people make with AFib?
Stopping blood thinners because they feel fine. AFib doesn’t always cause symptoms, but the stroke risk doesn’t disappear. Many people think, ‘If I don’t feel it, it’s not there.’ That’s dangerous. Others delay rhythm control too long, thinking it’s only for the severely ill. The truth? Early rhythm control improves survival. Don’t wait until you’re in the hospital to ask for better options.
Next Steps: What to Do Now
If you’ve been diagnosed with AFib, here’s your action plan:
- Get your CHA₂DS₂-VASc score calculated. If it’s 2 or higher, you need a blood thinner.
- Ask your doctor: ‘Am I a candidate for early rhythm control?’ Don’t accept ‘we’ll try rate control first’ without asking why.
- If you’re under 75 and symptomatic, request a referral to an electrophysiologist for ablation evaluation.
- Start lifestyle changes now: lose weight if needed, cut alcohol, treat sleep apnea, exercise regularly.
- Set reminders for your blood thinner. Missing doses is the #1 preventable cause of stroke in AFib.
AFib isn’t just a heart rhythm problem. It’s a life-altering condition. But with the right strategy, you don’t have to live with fear, fatigue, or the constant threat of stroke. The tools are here. The evidence is clear. Now it’s about choosing the right path-for your body, your life, and your future.






Vincent Soldja
December 2, 2025 AT 22:00Rate control works fine. Why complicate it with ablation? I’ve been on metoprolol for years. No strokes. No drama. Stop pushing procedures like they’re magic.
Katherine Gianelli
December 4, 2025 AT 00:41I know how scary AFib feels-you’re not alone. I had it for years and thought I just had to live with it until my cardiologist said ‘try rhythm control.’ Ablation wasn’t perfect, but after the second try, I finally slept through the night. No more panic when my heart skips. You deserve that peace too.
parth pandya
December 4, 2025 AT 21:17doac's are great but dont forget renal function! i had a friend on rivaroxaban and his creatinine spiked after 3 months. always check eGFR before prescribing. also ablation success drops hard if you have htn or sleep apnea. fix those first.
Makenzie Keely
December 5, 2025 AT 12:33Let me just say-this is one of the clearest, most compassionate breakdowns of AFib management I’ve ever read. Thank you. So many patients are told, ‘It’s just AFib, take a pill,’ and left to panic in silence. The fact that you included lifestyle changes as part of the treatment-not an afterthought-is revolutionary. And yes, stopping blood thinners because ‘you feel fine’? That’s like turning off your smoke alarm because the kitchen doesn’t smell like burning toast right now. Dangerous. Please, if you’re reading this: get your CHA₂DS₂-VASc score. Set phone alarms for your pills. Talk to an electrophysiologist. You’re not too old. You’re not too busy. Your future self will thank you.
Joykrishna Banerjee
December 7, 2025 AT 08:14Oh please. 'Early rhythm control saves lives'? That's EAST-AFNET 4 cherry-picked by Big Pharma and overzealous EPs. The absolute risk reduction was 3.9%-which means 25 people need to be ablated to prevent one event. Meanwhile, the cost? $30K per procedure. And let's not forget the 5% complication rate-stroke, tamponade, esophageal fistula. Meanwhile, rate control costs $20/month. You're being sold a luxury, not a lifeline. Also, DOACs? They're not 'better.' They're just more expensive. Warfarin has been around since 1954. If it ain't broke...
Gene Linetsky
December 7, 2025 AT 21:13They don't want you to know this but the real reason they push ablation is because the hospitals make 10x more money off it than prescribing metoprolol. And don't get me started on DOACs-those are just fancy pills made by the same companies that sold you OxyContin. They're not curing you. They're just keeping you hooked. Wake up. The system is rigged.
Chloe Madison
December 9, 2025 AT 19:59To the person who said ‘rate control is enough’-I hear you. I was you. But after 18 months of being too tired to play with my kids, I asked for ablation. It wasn’t easy. Recovery sucked. But now? I hiked 8 miles last weekend. No fluttering. No fear. I didn’t ‘give up’ on rate control-I upgraded. And if you’re hesitating because you think it’s too late? It’s not. You’re not too old. You’re not too late. Your heart still wants to beat right. Let it.
Francine Phillips
December 11, 2025 AT 11:02My dad had AFib. They put him on warfarin. He forgot to take it. Had a stroke. He’s fine now but he can’t walk right. I just wish someone had told us earlier that skipping pills is the #1 mistake. Just set a reminder. Please.
Myson Jones
December 11, 2025 AT 21:08Thank you for this comprehensive overview. It is evident that the evolution of AFib management has been profoundly influenced by robust clinical evidence, particularly the EAST-AFNET 4 trial, which substantiates the superiority of early rhythm control in reducing composite cardiovascular events. Furthermore, the emphasis on DOACs as first-line anticoagulants aligns with contemporary guidelines from both the ACC and ESC. It is imperative that clinicians move beyond entrenched practice patterns and adopt patient-centered, evidence-based decision-making frameworks. Lifestyle modifications, including weight loss and sleep apnea treatment, must be integrated into therapeutic algorithms as non-pharmacological pillars of care. The future of AFib management lies not in passive surveillance, but in proactive restoration of sinus rhythm-when indicated-with concomitant risk factor modification. This paradigm shift is not merely prudent; it is ethically obligatory.