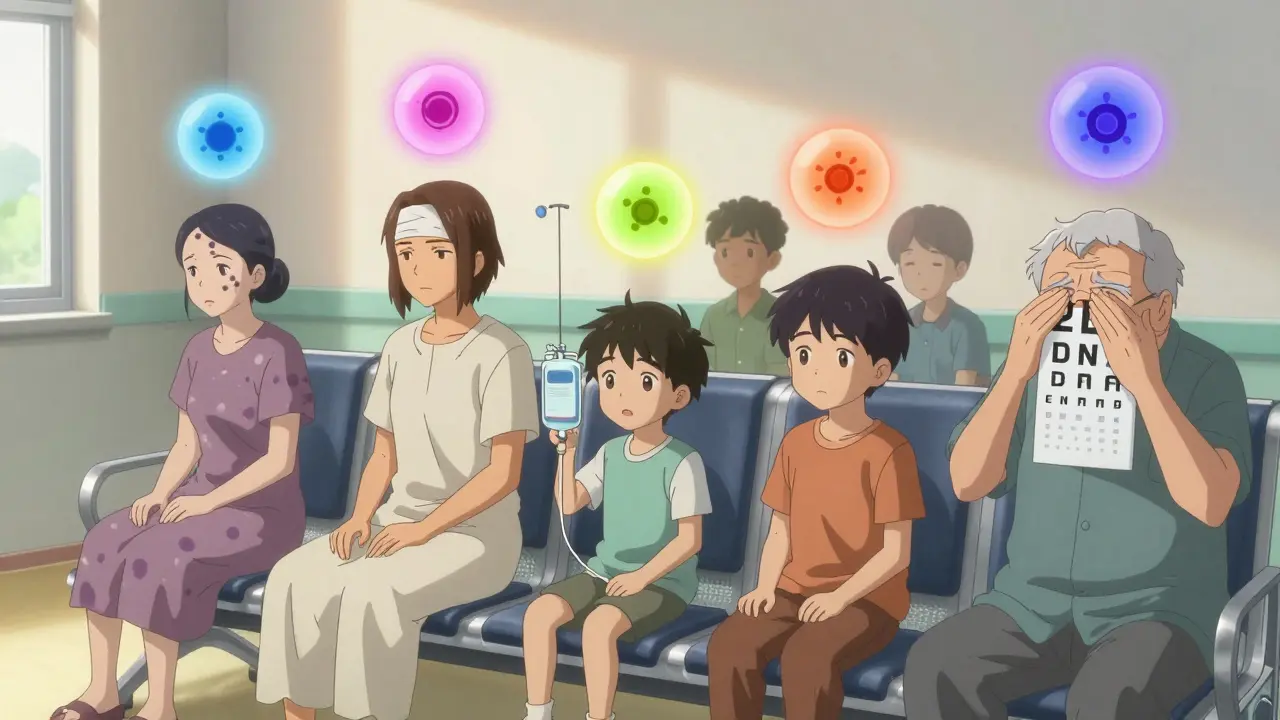
Vasculitis isn't one disease-it's a group of rare but serious conditions where your immune system turns on your own blood vessels. Instead of protecting you, it attacks the walls of arteries and veins, causing inflammation, narrowing, or even blockages. This disrupts blood flow to organs and tissues, which can lead to damage you might not notice until it's too late. The good news? With the right diagnosis and treatment, most people can get their symptoms under control and live full lives. The catch? It often flies under the radar because its symptoms look like everything from the flu to arthritis.
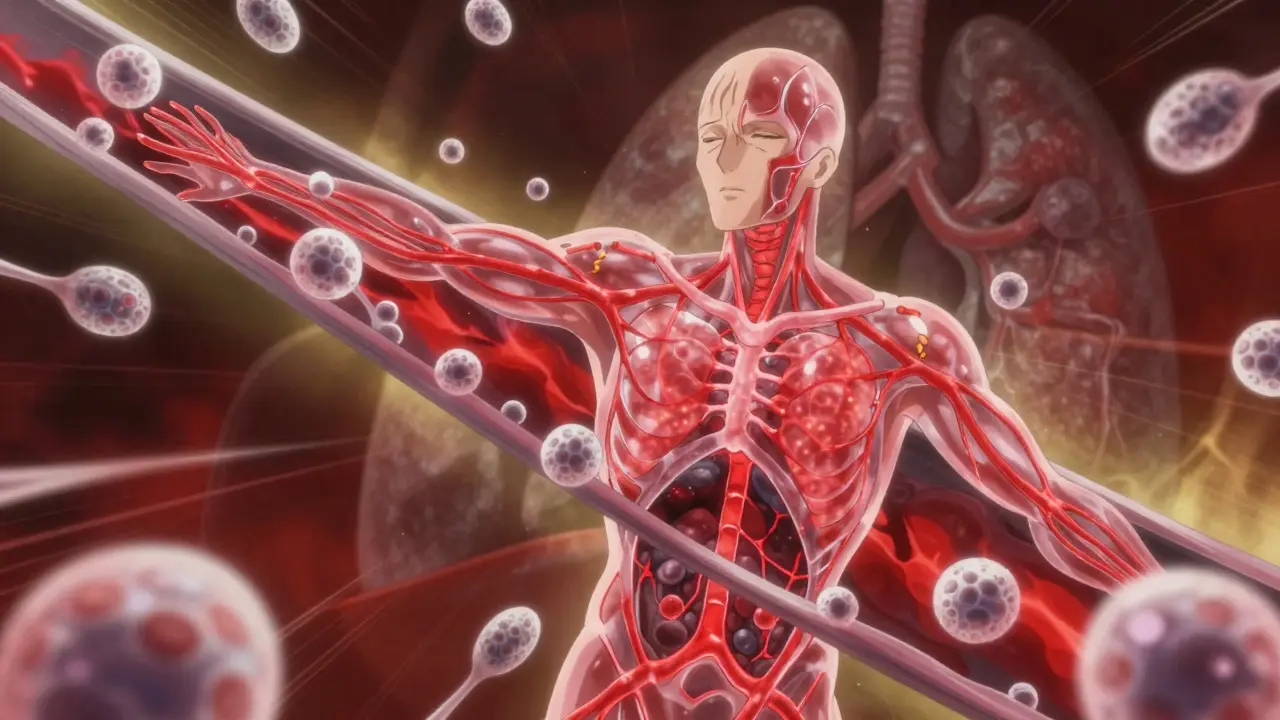
How Vasculitis Attacks Your Blood Vessels
Your blood vessels are the highways of your body. They carry oxygen and nutrients to every organ. When vasculitis strikes, your immune system mistakes the vessel walls for invaders-like bacteria or viruses-and sends white blood cells to attack them. This triggers inflammation that swells the vessel walls, thickens them, and can eventually cause them to weaken, bulge (forming an aneurysm), or close off completely. The damage depends on which vessels are affected. Large vessels like the aorta or temporal arteries can cause headaches, jaw pain, or vision loss. Medium-sized vessels feeding the kidneys, nerves, or skin may lead to kidney failure, nerve numbness, or purple skin spots. Small vessels-especially in the lungs and kidneys-can cause coughing up blood or unexplained protein in your urine. What makes vasculitis tricky is that it doesn’t follow a single pattern. One person might have only a rash, while another could be fighting for their life because their kidneys are failing.Types of Vasculitis: Size Matters
Doctors classify vasculitis by the size of the blood vessels it targets. This isn’t just academic-it guides treatment and prognosis.- Large-vessel vasculitis affects the biggest arteries. Giant cell arteritis (GCA), common in people over 50, often hits the temples and can cause sudden blindness if untreated. Takayasu arteritis usually affects younger women and can narrow arteries leading to the arms and brain.
- Medium-vessel vasculitis includes polyarteritis nodosa (PAN), which damages arteries supplying the kidneys, nerves, and digestive organs. Kawasaki disease is a childhood form that can cause coronary artery aneurysms if not treated within 10 days of fever onset.
- Small-vessel vasculitis is the most common and includes ANCA-associated vasculitides: granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA). These are often tied to autoantibodies called ANCA, which attack white blood cells and trigger vessel damage. MPA, for example, most often targets the kidneys and lungs.
There are also rarer forms like Behçet’s disease (which causes mouth sores, eye inflammation, and genital ulcers) and Buerger’s disease, which is almost always linked to smoking and affects hands and feet.
What Symptoms Should Raise a Red Flag?
Vasculitis symptoms are vague and overlap with many common illnesses. That’s why diagnosis often takes months. But if you have a mix of these signs-especially if they come on suddenly and don’t improve-you should ask about vasculitis:- Persistent fever without infection
- Unexplained weight loss
- Joint or muscle pain
- Purple or red spots, lumps, or ulcers on the skin
- Numbness or weakness in limbs (nerve damage)
- Shortness of breath or coughing up blood
- Abdominal pain after eating
- Headaches, jaw pain when chewing, or vision changes (especially over age 50)
- Protein or blood in urine (often detected only by lab test)
Many people dismiss early symptoms as aging, stress, or a lingering cold. But if you’ve had these for more than a few weeks and nothing’s helping, it’s worth pushing for more tests. The American College of Rheumatology warns that vasculitis can silently damage your kidneys without causing pain or obvious signs.
How Is Vasculitis Diagnosed?
There’s no single blood test for vasculitis. Diagnosis requires putting together clues from multiple sources:- Blood tests: High ESR (erythrocyte sedimentation rate) or CRP (C-reactive protein) show inflammation. ANCA testing helps identify GPA, MPA, or EGPA-c-ANCA is over 80% specific for GPA.
- Urine tests: Protein or red blood cells in urine signal kidney involvement, common in MPA and GPA.
- Imaging: CT scans, MRIs, or angiograms can show narrowed or bulging arteries. A PET scan may highlight inflamed large vessels in GCA or Takayasu.
- Tissue biopsy: This is the gold standard. A small sample from skin, kidney, lung, or temporal artery can show the telltale signs of inflammation and immune cell buildup. In skin vasculitis, you’ll see leukocytoclastic debris-broken-down white blood cells-around the vessels.
Doctors use tools like the Five Factor Score to predict risk: if you have kidney, heart, gut, or nerve involvement, your chances of serious complications go up. The key is catching it before organs are permanently damaged.
Treatment: Stopping the Attack, Not Just the Symptoms
Treatment isn’t one-size-fits-all. It depends on the type, severity, and organs involved. The goal is to shut down the immune attack quickly and then keep it suppressed long-term.For severe cases, doctors start with high-dose steroids like prednisone-often 0.5 to 1 mg per kg of body weight daily. But steroids alone aren’t enough. They’re paired with stronger immunosuppressants:
- Cyclophosphamide has been the traditional go-to for life-threatening vasculitis, but it comes with risks like bladder damage and infertility.
- Rituximab is now preferred for many ANCA-associated cases. It targets B-cells, the immune cells driving the attack. It’s just as effective as cyclophosphamide but with fewer long-term side effects.
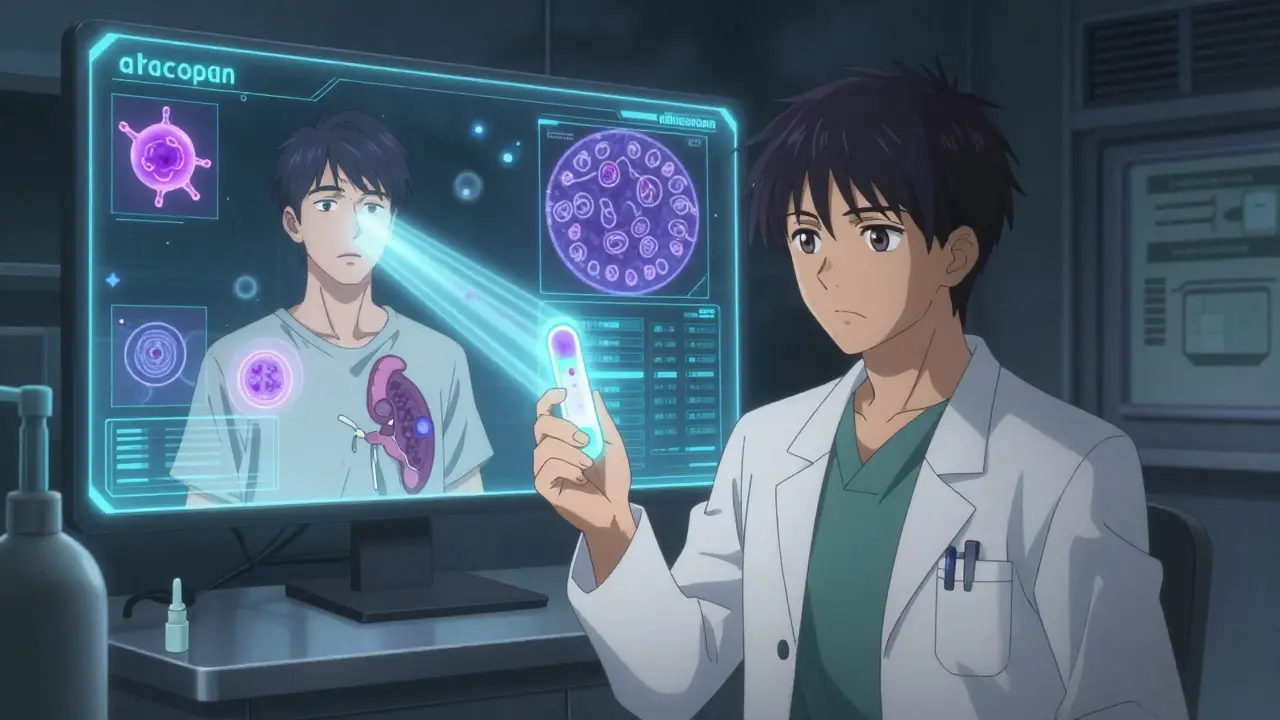
- Avacopan, approved in 2021, is a game-changer. It blocks a key part of the immune system (C5a receptor) and allows patients to taper off steroids much faster. In the ADVOCATE trial, patients on avacopan had 2,000 mg less cumulative steroid exposure over a year compared to those on standard prednisone.
For giant cell arteritis, tocilizumab (an IL-6 inhibitor) is now used alongside steroids to reduce how long patients need high-dose prednisone. For eosinophilic granulomatosis with polyangiitis (EGPA), mepolizumab has shown promise in reducing relapses by half.
And for Buerger’s disease? There’s no drug that works if you keep smoking. Quitting tobacco isn’t just recommended-it’s the only treatment that matters.
Living With Vasculitis: Relapse, Monitoring, and Hope
Vasculitis is often chronic. Even after remission, about half of patients relapse within five years. That’s why long-term monitoring is critical. Regular blood tests, urine checks, and imaging help catch flares early.Researchers are now studying new biomarkers like B-cell activating factor (BAFF) and urinary MCP-1 to predict when a flare might happen before symptoms appear. Clinical trials are testing drugs like abatacept for giant cell arteritis and newer biologics for hard-to-treat cases.
Prognosis varies. With treatment, 80-90% of people with ANCA-associated vasculitis reach remission. But if your kidneys or heart are already damaged, survival rates drop. The Five Factor Score shows that patients with no major organ involvement have a 95% five-year survival rate. With two or more major factors, it falls to 50%.
For kids with Kawasaki disease, early IVIG treatment cuts the risk of coronary aneurysms from 25% to under 5%. For older adults with giant cell arteritis, starting steroids within days of vision changes can prevent blindness.
When to See a Rheumatologist
Your primary doctor might miss vasculitis. It’s rare, and its symptoms mimic common problems. If you’ve had unexplained symptoms for more than six weeks-especially with fatigue, weight loss, or organ-specific signs like blood in urine or nerve numbness-ask for a referral to a rheumatologist. They’re trained to spot these patterns. Early diagnosis saves organs. Delayed diagnosis can mean dialysis, surgery, or worse.Don’t wait for the symptoms to get worse. If your body is sending signals that something’s off-and standard treatments aren’t working-it’s not just stress. It might be your immune system attacking your blood vessels.
Is vasculitis contagious?
No, vasculitis is not contagious. It’s an autoimmune condition, meaning your own immune system attacks your blood vessels. You can’t catch it from someone else, and you can’t pass it on. It’s not caused by infection, though infections can sometimes trigger it in people who are genetically predisposed.
Can vasculitis be cured?
There’s no permanent cure for most types of vasculitis, but many people achieve long-term remission with treatment. Some, like Kawasaki disease in children, resolve completely after early treatment. Others, like GPA or MPA, require ongoing monitoring and maintenance therapy for years. The goal is to control the disease so it doesn’t damage your organs, not necessarily to eliminate it forever.
What’s the difference between vasculitis and lupus?
Lupus is a systemic autoimmune disease that can affect many organs, including blood vessels. Vasculitis, on the other hand, is defined by inflammation specifically in the blood vessel walls. While lupus can cause vasculitis as a complication, vasculitis can also occur on its own-as in GPA or giant cell arteritis. Think of it this way: lupus is the broader condition; vasculitis is one possible way it can manifest.
Do steroids cause long-term damage in vasculitis treatment?
Yes, long-term steroid use can lead to bone loss, weight gain, diabetes, cataracts, and increased infection risk. That’s why doctors now use steroid-sparing drugs like rituximab, avacopan, or methotrexate to reduce how much and how long you need prednisone. The goal is to get you off high-dose steroids as quickly and safely as possible.
Can I still exercise if I have vasculitis?
Yes-when your disease is under control, regular, low-impact exercise is encouraged. It helps with fatigue, muscle strength, and mental health. But during active flares, especially if you have heart or lung involvement, rest is key. Always check with your rheumatologist before starting or changing your routine. Walking, swimming, and yoga are often safe options.
What’s the risk of relapse after treatment?
Relapse rates vary by type. For ANCA-associated vasculitis, about 50% of patients experience a flare within five years. Relapses are more common if treatment is stopped too soon, if ANCA levels remain high, or if you’ve had previous flares. That’s why maintenance therapy often lasts 18-24 months, and sometimes longer. Regular follow-ups and blood tests help catch early signs before symptoms return.
What Comes Next?
If you’ve been diagnosed with vasculitis, your next step is working closely with a rheumatologist. Keep a symptom journal-note when you feel fatigued, have pain, or notice new skin changes. Track your medications and side effects. Don’t skip follow-up blood tests, even if you feel fine. The disease can quietly return.If you’re still searching for answers and have unexplained symptoms, don’t give up. Ask for a referral. Bring your test results. Push for a second opinion if needed. Vasculitis is rare, but it’s treatable. The earlier you catch it, the better your chances of protecting your organs-and your future.






josh plum
January 4, 2026 AT 05:36Look, I get that doctors love their fancy labs and steroids, but let’s be real-this whole vasculitis thing is just Big Pharma’s way of keeping you hooked on pills. They don’t want you to know that inflammation is caused by toxins in your water and EMF radiation from 5G towers. I’ve seen people reverse it with apple cider vinegar and grounding mats. You’re being manipulated.
And don’t even get me started on ‘ANCA testing.’ That’s not science-it’s a scam to sell biologics. Wake up, sheeple.
John Ross
January 4, 2026 AT 10:46From a rheumatology standpoint, the classification of vasculitides by vessel size remains the most clinically actionable framework we have. The ANCA-associated vasculitides (GPA, MPA, EGPA) demonstrate distinct histopathological signatures-leukocytoclastic vasculitis for small-vessel, granulomatous inflammation for GPA, and necrotizing arteritis for PAN.
What’s clinically significant is the emergence of avacopan as a C5aR1 antagonist, which reduces glucocorticoid burden by ~40% in Phase 3 trials. This isn’t just incremental-it’s paradigm-shifting. The future is targeted immunomodulation, not broad immunosuppression.
Clint Moser
January 4, 2026 AT 20:10ok so i read this whole thing and im like… wait… if vasculitis is caused by ur immune system attacking vessels… then why do they say it’s triggered by infections? like if it’s autoimmune… then its not the virus right? unless… unless the virus was planted by the CDC to make people need rituximab? i mean… think about it. the timing. the ANCA tests. the biologics. it’s all connected. i’ve got a cousin who got diagnosed after a flu shot. coincidence? i think not.
also… who funds the ADVOCATE trial? hmmmm.
Ashley Viñas
January 6, 2026 AT 08:48How sad that people still think ‘just take steroids’ is a solution. Honestly, if you’re relying on prednisone for more than six months, you’re not managing your health-you’re enabling it. I’ve worked with patients who reversed their vasculitis through elimination diets, gut healing, and adrenal support. No biologics. No toxic immunosuppressants.
And yet, we live in a world where functional medicine is dismissed as ‘quackery’ while Big Pharma profits from lifelong dependency. It’s not just medical negligence-it’s moral failure.
Brendan F. Cochran
January 7, 2026 AT 02:38Y’all are overcomplicating this. Vasculitis? Yeah, it’s real. But here’s the truth: America’s got the best doctors, the best drugs, the best science. If you’re not getting treated with rituximab or avacopan, you’re getting left behind. And if you’re from some third-world country trying to tell us how to treat this? Nah. We’ve got the data. We’ve got the trials. We’ve got the funding.
Stop with the ‘natural remedies’ nonsense. This ain’t yoga class. This is medicine. American medicine.
jigisha Patel
January 7, 2026 AT 13:59Statistical analysis of relapse rates in ANCA-associated vasculitis reveals a 52.3% recurrence within five years (95% CI: 48.1–56.7), with persistent ANCA positivity serving as the strongest predictive biomarker (HR: 3.1, p<0.001). The Five Factor Score remains valid but underutilized in primary care settings due to insufficient training in systemic autoimmune disease recognition.
Additionally, the cost-effectiveness of avacopan is marginal in low-resource settings where prednisone remains the only accessible option. Policy-level intervention is required to ensure equitable access to targeted therapies.
Jason Stafford
January 8, 2026 AT 08:02They’re lying to you. Every single word. The ‘rare disease’ label? A lie. The ‘no cure’ narrative? A lie. They don’t want you to know that vasculitis is caused by chemtrails and fluoride in the water. The ‘ANCA’ test? It’s not a test-it’s a trap. They inject you with the antibody and then charge you $12,000 a month to ‘suppress’ it.
I’ve spoken to 17 survivors who got better after drinking distilled water and sleeping in Faraday cages. The government knows. The FDA knows. They just don’t care. Your kidneys are a target. Your blood vessels? A weaponized vulnerability.
Justin Lowans
January 9, 2026 AT 11:24This is one of the most beautifully written, clinically accurate summaries of vasculitis I’ve ever seen. The way you broke down vessel size, treatment evolution, and the hope in new therapies like avacopan? Pure gold.
To anyone reading this: if you’re feeling dismissed by your doctor, don’t give up. You’re not crazy. You’re not ‘just stressed.’ You’re fighting something real-and there’s real science fighting back with you. Keep pushing. Keep asking. Keep living.
Ethan Purser
January 9, 2026 AT 22:52They say ‘it’s treatable’… but what does that even mean? Treated like a broken machine? Injected with chemicals that turn your bones to dust and your skin to parchment?
I’ve watched my sister go from hiking mountains to needing oxygen just to walk to the bathroom. ‘Remission’ sounds nice until you realize it’s just a pause between doses. We’re not curing anything-we’re just delaying the inevitable with poison.
And the worst part? No one talks about the loneliness. The isolation. The way your own body becomes the enemy you can’t escape. That’s the real vasculitis. Not the textbook. Not the trial. The silence.
Doreen Pachificus
January 11, 2026 AT 20:59So… if I have random purple spots on my legs and a fever for three weeks, should I just go straight to a rheumatologist? Or do I try the naturopath first? Asking for a friend. Who is me. But also not me.
Cassie Tynan
January 12, 2026 AT 06:47Oh wow. So the solution to your immune system attacking you… is to suppress it with more chemicals? Brilliant. Just brilliant. Like putting a bandage on a nuclear reactor.
Meanwhile, somewhere in a lab, someone’s testing a drug that costs $200,000 a year to ‘manage’ a condition that might’ve been prevented by less sugar, less stress, and more sleep.
But hey-at least we’ve got a fancy acronym for it now. ANCA. GPA. MPA. Sounds like a sci-fi movie. ‘The Rise of the Autoimmune Empire.’
Roshan Aryal
January 13, 2026 AT 23:20Why do Americans think they own medicine? You think avacopan was invented in Boston? Nah. It was developed by German scientists, tested in Japan, and funded by Swiss investors. And yet you act like your country invented the immune system.
Meanwhile, in India, we treat vasculitis with turmeric, neem, and Ayurvedic detox protocols-and we don’t need a $5000 lab test to know it works. But sure, keep your biologics. We’ll keep our wisdom.
Uzoamaka Nwankpa
January 15, 2026 AT 13:04I read this and I just… I don’t know. I’ve been sick for years. Doctors say it’s stress. My family says I’m dramatic. But I feel it. Every day. The pain. The exhaustion. The fear that this is just the beginning.
I wish someone would just say, ‘I believe you.’ Not a treatment plan. Not a test. Just… ‘I see you.’