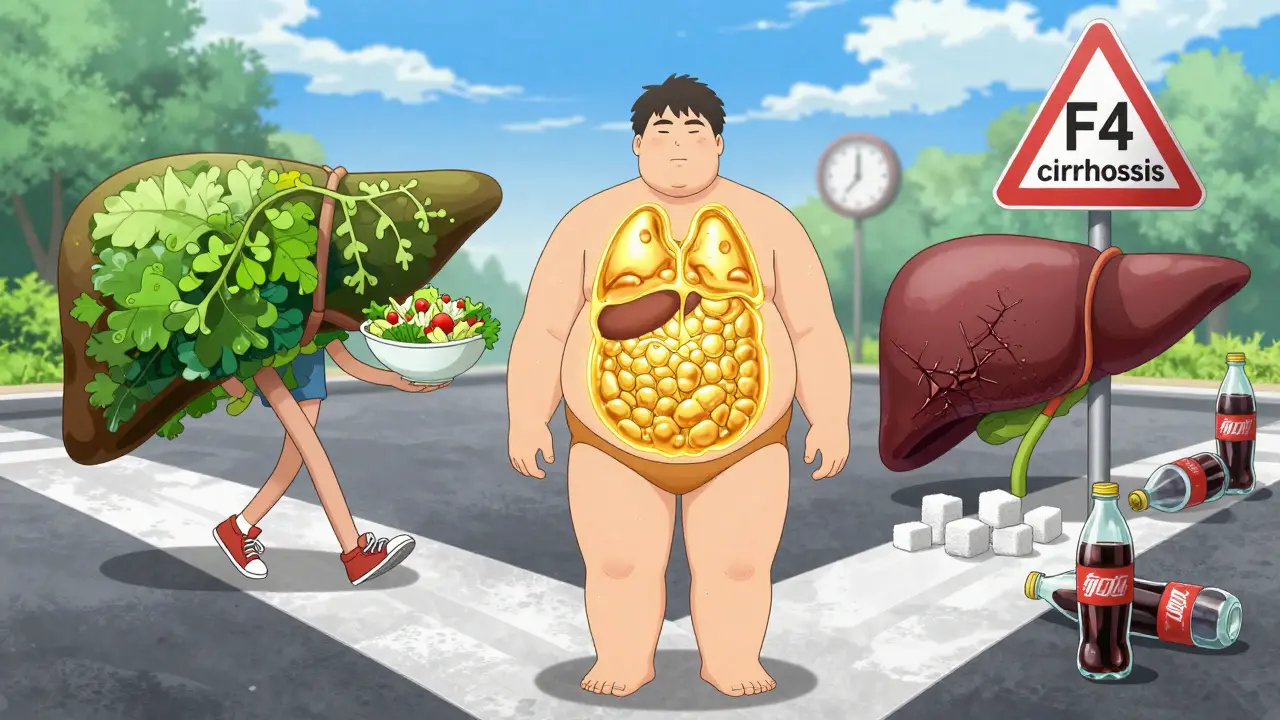
Most people with fatty liver don’t feel sick. No pain. No warning signs. Just a routine blood test that shows slightly elevated liver enzymes-and suddenly, you’re told you have NAFLD. But what does that really mean? Is it just fat in the liver, or is something more dangerous happening? The difference between NAFLD and NASH isn’t just medical jargon-it’s the line between a manageable condition and one that could lead to cirrhosis, liver cancer, or even death.
What’s the Difference Between NAFLD and NASH?
NAFLD stands for Non-Alcoholic Fatty Liver Disease. It’s not caused by drinking alcohol. Instead, it’s linked to how your body handles sugar, fat, and insulin. Think of NAFLD as a big umbrella. Under it, there are two main conditions: simple fatty liver (called NAFL) and the more serious form, NASH.
NAFL means you have fat building up in your liver-5% or more of its weight-but no inflammation or damage to liver cells. It’s like having a garage full of old boxes. Not ideal, but not actively breaking anything. Most people with NAFL never develop serious problems. A 15-year study of over 1,200 people found only about 12% of them progressed to significant liver scarring.
NASH, on the other hand, is when that fat starts to cause trouble. Liver cells swell (called ballooning), immune cells attack, and inflammation kicks in. This isn’t just storage anymore-it’s damage. And with damage comes fibrosis: scar tissue replacing healthy liver. That’s the real danger. NASH can quietly turn into cirrhosis, liver failure, or hepatocellular carcinoma. About 40% of people with NASH develop advanced fibrosis over 10-20 years.
Fibrosis: The Silent Progression
Fibrosis is measured on a scale from F0 to F4. F0 means no scarring. F1 and F2 are mild to moderate. F3 is bridging fibrosis-scar tissue starts connecting across liver zones. F4 is cirrhosis: the liver is hardened, shrunken, and struggling to function.
The scary part? You can have F3 fibrosis and still feel fine. No jaundice. No swelling. Just fatigue you blame on stress. That’s why liver biopsy remains the gold standard for diagnosis-it’s the only way to confirm NASH and accurately stage fibrosis. But it’s invasive. So doctors use tools like FibroScan, which measures liver stiffness, or blood tests like FIB-4, which combines your age, platelet count, and liver enzyme levels.
Here’s what matters: if your FIB-4 score is above 1.3, you’re at risk for advanced fibrosis. Above 2.67? You need a specialist. A FibroScan reading over 7.1 kPa suggests significant scarring. Over 10 kPa? That’s a red flag for cirrhosis.
Who’s at Risk?
NAFLD and NASH aren’t random. They’re tied to metabolic health. If you have three or more of these, you’re in the high-risk zone:
- Waist size over 40 inches (men) or 35 inches (women)
- BMI of 30 or higher
- High blood pressure (130/85 or more)
- Triglycerides above 150 mg/dL
- Fasting blood sugar over 100 mg/dL
That’s metabolic syndrome. And it’s the engine behind NASH. About 70-90% of NASH patients are obese. Half have type 2 diabetes. Two-thirds have high blood pressure. Even sleep apnea is a red flag-30-50% of NASH patients have it.
It’s not just about weight, though. Even people with normal BMI can develop NASH if they have insulin resistance or carry fat around their organs. That’s why doctors now look at your entire metabolic picture-not just your scale.

Diagnosis: What Tests Actually Matter?
Many people get diagnosed after a routine blood test shows high ALT or AST. Normal ALT is 7-55 U/L. If yours is 68, like one Reddit user found, that’s a signal. But blood tests alone can’t tell you if it’s NAFL or NASH. That’s where imaging comes in.
Ultrasound can spot fat if it’s over 20-30% of the liver. But it misses mild cases. MRI-PDFF is better-95% accurate at measuring fat content. But it’s expensive and not widely available.
That’s why most doctors start with FIB-4 or FibroScan. If those suggest advanced fibrosis, they’ll refer you for a biopsy. The biopsy isn’t perfect-it can miss damage because liver tissue varies. But it’s still the only way to confirm NASH.
And here’s a reality check: up to 30% of people told they have NASH based on blood or scan results don’t actually have it on biopsy. That’s why experts warn against overdiagnosis. Don’t panic over a single test. Wait for confirmation.
What Happens If You Do Nothing?
NAFL? Your risk of liver death is very low-under 1% over 10 years. But NASH? That jumps to 12-25% if you have F3 or F4 fibrosis. And while liver disease is the main concern, most people with NASH die from heart disease. About 42% of deaths in NAFLD patients are from cardiovascular causes.
But the real threat is progression. NASH can turn into cirrhosis in 10-20 years. And once cirrhosis sets in, your risk of liver cancer rises sharply. About 5-12% of NASH patients develop hepatocellular carcinoma. That’s why early detection matters more than ever.
Can You Reverse It?
Yes. And that’s the most important thing to know.
Weight loss is the most powerful tool. Losing just 5% of your body weight can reduce liver fat. Lose 7-10%, and you can reverse NASH entirely. One patient on a support forum lost 10% of his weight in 18 months and went from NASH back to simple fatty liver.
It’s not magic. It’s metabolic reset. Cut sugary drinks. Reduce refined carbs. Move daily-even walking 30 minutes helps. Studies show that people who lose weight and keep it off have an 85% chance of improving fibrosis.
There’s also new hope. In March 2023, the FDA approved resmetirom (Rezdiffra), the first drug specifically for NASH with moderate to advanced fibrosis. In trials, it improved fibrosis in 26% of patients versus 10% on placebo. More drugs are in phase 3 trials. But right now, lifestyle is still the only proven treatment for most people.
The Big Shift: MASLD and MASH
In June 2023, major liver societies dropped NAFLD and NASH. They’re now called MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease) and MASH (Metabolic Dysfunction-Associated Steatohepatitis).
Why? Because “non-alcoholic” was misleading. It made people think it was about what they didn’t drink, not what they did have: insulin resistance, obesity, high blood sugar. The new names focus on the root cause-metabolic dysfunction.
It’s not just semantics. It’s about reducing stigma and improving care. If you’re told you have MASLD, it means your liver is reacting to how your body handles energy-not because you drank too much.
What Should You Do Now?
If you’ve been told you have fatty liver:
- Don’t ignore it. Even if you feel fine, get your FIB-4 score checked.
- Ask for a FibroScan if your doctor hasn’t offered one.
- Get your blood sugar, cholesterol, and blood pressure checked.
- Start losing weight-5% is a good first goal.
- Avoid alcohol, even if you’re told it’s “non-alcoholic” liver disease. It adds stress.
- See a hepatologist if you have advanced fibrosis or diabetes.
If you’re healthy but overweight or have prediabetes, get screened. One blood test could catch this before it turns into something serious.
The liver is quiet until it’s not. But unlike many diseases, this one responds to action. The earlier you change, the better your chances. You don’t need a miracle drug. You need to eat better, move more, and take your metabolic health seriously.
Can you have NASH without being overweight?
Yes. While most people with NASH are overweight or obese, about 10-20% have normal BMI. These are often called "lean NASH" cases. The key factor isn’t weight-it’s insulin resistance and fat stored around internal organs. Genetics, diet, and gut health also play roles. A person with normal weight but high triglycerides, high blood sugar, or low HDL can still develop NASH.
Is a liver biopsy always necessary to diagnose NASH?
No. Most people don’t need one. Doctors use non-invasive tools like FibroScan, FIB-4, and MRI-PDFF to assess risk. Biopsy is only recommended if those tests suggest advanced fibrosis (F3 or F4), or if there’s uncertainty about the diagnosis. It’s invasive and carries small risks, so it’s reserved for cases where treatment decisions depend on knowing the exact stage of liver damage.
Can NAFLD turn into liver cancer?
Directly, NAFLD doesn’t cause cancer. But if it progresses to NASH and then to cirrhosis, the risk of hepatocellular carcinoma (HCC) increases sharply. About 5-12% of NASH patients develop liver cancer over time. Even without cirrhosis, some studies show a slightly higher risk of HCC in NASH patients-so monitoring is still important.
Are there any medications for NAFLD or NASH?
As of late 2025, resmetirom (Rezdiffra) is the first FDA-approved drug for NASH with moderate to advanced fibrosis. It targets liver metabolism and has shown fibrosis improvement in clinical trials. Other drugs are in phase 3 testing. But for most people, no medication replaces lifestyle change. Weight loss, exercise, and managing diabetes and cholesterol remain the foundation of treatment.
How often should I get checked if I have NAFLD?
If you have simple fatty liver (NAFL) and no other risk factors, check liver enzymes and metabolic markers every 1-2 years. If you have NASH or fibrosis, you should be seen by a specialist every 6-12 months. Those with advanced fibrosis (F3-F4) need annual monitoring for liver cancer, including ultrasound and AFP blood tests.






Jeffrey Frye
December 24, 2025 AT 05:22so i got my alt at 68 last month and immediately panicked. google told me i was gonna die by 40. then i found out my buddy who eats nothing but pizza and energy drinks has an alt of 72 and runs marathons. so yeah. maybe stop doomscrolling and get a fib-4?
claire davies
December 25, 2025 AT 18:16okay but can we talk about how the term 'non-alcoholic' always felt like a cop-out? like, oh you didn't drink, so it's fine? nope. it's about how your body handles sugar like it's a personal insult. i love that they renamed it MASLD-finally, the name reflects the real villain: metabolic dysfunction. also, if you're reading this and think 'but i'm thin!'-sweetie, i had lean NASH. my waist was 28 inches, my visceral fat was screaming. it's not about the scale. it's about the insulin resistance hiding in your liver like a ghost. get your fasting insulin checked. please.
Lindsey Kidd
December 26, 2025 AT 13:17thank you for this. 🙏 i was diagnosed last year and thought i was doomed. lost 12% in 8 months with walking + cutting soda. fibroscan went from 9.8 to 6.2. it’s not magic. it’s just not giving your liver a reason to cry anymore. 🍎🚶♀️
Usha Sundar
December 27, 2025 AT 12:20my dad had cirrhosis. he ignored it for 7 years. don’t be him.
Rosemary O'Shea
December 27, 2025 AT 14:50How quaint. You all treat this like it’s a lifestyle blog. Have any of you read the 2024 Lancet meta-analysis on fibrosis progression in metabolically healthy obese individuals? Or the recent paper on gut-liver axis dysbiosis in lean NASH? No? Then perhaps you should stop offering anecdotal ‘remedies’ and acknowledge that this is a complex, multi-system metabolic disorder-not a ‘lose 5% and you’re fine’ wellness hack. The pharmaceutical industry is finally catching up, and yet, the Reddit wisdom persists. Sigh.
Abby Polhill
December 28, 2025 AT 05:50the fib-4 >2.67 threshold is such a useful cutoff-but i’ve seen so many patients get dismissed because their bmi is ‘normal.’ lean NASH is real, and it’s underdiagnosed because we’re still stuck in the obesity-centric paradigm. also, apolipoprotein B >130 is a better predictor than triglycerides in some cases. just saying.
Raja P
December 28, 2025 AT 14:59just wanna say thanks to everyone sharing. i’ve been scared to even look at my bloodwork for a year. reading this made me call my doc today and ask for a fibroscan. small step, but it’s a step.
Spencer Garcia
December 29, 2025 AT 07:13if you’re on metformin and have NAFLD, keep taking it. it helps. also, walking after meals lowers postprandial glucose spikes. 10 mins after dinner > 10 mins on a treadmill at 7pm.
Joseph Manuel
December 29, 2025 AT 20:23While the article presents a compelling overview of MASLD/MASH pathophysiology, it is methodologically flawed in its reliance on non-invasive biomarkers as diagnostic proxies for histological confirmation. The sensitivity of FIB-4 for advanced fibrosis is approximately 78%, with a specificity of 82%-insufficient for clinical decision-making without biopsy validation. Furthermore, the assertion that weight loss alone can reverse NASH is overstated; only 30-40% of patients achieve histological improvement without concomitant pharmacotherapy. The approval of resmetirom represents a paradigm shift, and its integration into clinical guidelines must be prioritized over lifestyle recommendations alone.
Delilah Rose
December 30, 2025 AT 09:02i read this whole thing and cried a little. not because i’m scared-but because i finally get it. i thought my fatigue was just ‘mom life.’ my high triglycerides? ‘genetics.’ my belly fat? ‘just how i’m built.’ but it’s all connected. i’m 41, have prediabetes, and my fib-4 is 1.8. i didn’t know what to do. now i do. i’m starting with cutting out the midnight ice cream. and yes, i’m asking for a fibroscan. thank you for not making me feel like a failure. this isn’t about willpower. it’s about biology. and i’m ready to learn.