Drug Interaction Checker for Acid-Reducing Medications
Enter your medication name to see if it interacts with acid-reducing drugs like omeprazole, famotidine, or other heartburn medications. This tool is based on FDA guidelines and research findings from the article.
Many people take acid-reducing medications like omeprazole or famotidine for heartburn or stomach ulcers. But few realize these common drugs can quietly wreck the effectiveness of other medications they’re taking. It’s not a rare side effect - it’s a well-documented, widespread problem that affects thousands of patients every year. If you’re on a pill for HIV, leukemia, or even a fungal infection, your heartburn medicine could be making it useless.
How Acid-Reducing Drugs Work - And Why That Matters
Proton pump inhibitors (PPIs) like omeprazole, esomeprazole, and lansoprazole, and H2 blockers like ranitidine and famotidine, reduce stomach acid by targeting different parts of the acid-production system. PPIs shut down the final step - the proton pump in stomach cells - and their effect lasts 14 to 18 hours a day. H2 blockers work faster but only last 8 to 12 hours. Both raise stomach pH from its normal acidic level of 1-3.5 up to 4-6. That sounds harmless, even helpful. But it changes how your body absorbs many other drugs. Most oral medications don’t get absorbed in the stomach. About 90% of absorption happens in the small intestine, where the pH is around 6-8. But for many drugs, the journey starts in the stomach. If they can’t dissolve properly there, they never make it to where they’re absorbed. And dissolution depends on pH.The Science Behind the Interference
Drugs are either weak acids or weak bases. Weak bases - like atazanavir, dasatinib, and ketoconazole - need an acidic environment to dissolve. In a normal stomach, they become charged and soluble. When you take a PPI, the stomach becomes less acidic, and these drugs stay neutral. They don’t dissolve. They just sit there, pass through the gut, and get excreted. No absorption. No effect. A 2022 study from Celerion found that when atazanavir (an HIV drug) is taken with lansoprazole, its absorption drops by 95%. That’s not a small drop. That’s treatment failure. The FDA lists atazanavir as one of the highest-risk drugs for this interaction. Patients on this combo have seen their viral load spike from undetectable to over 12,000 copies/mL - all because they started omeprazole for heartburn. Weak acids like aspirin behave differently. They dissolve better in higher pH, so their absorption might increase slightly. But that’s rarely a problem. The real danger is with weak bases - especially those with a narrow therapeutic index. That means the difference between a helpful dose and a toxic one is tiny. Even a 20% drop in absorption can mean the drug stops working.Which Drugs Are Most at Risk?
The FDA has flagged 12 high-risk drugs affected by acid-reducing medications. Here are the big ones:- Atazanavir (HIV treatment): 74-95% drop in absorption with PPIs. Never combine.
- Dasatinib (leukemia drug): 60% reduction. Dose adjustments or staggered timing may help.
- Ketoconazole (antifungal): 75% drop. Often becomes completely ineffective.
- Nilotinib (another leukemia drug): 40-60% reduced absorption.
- Myfortic (mycophenolate mofetil): Used after transplants. Absorption drops significantly.
- Eliglustat (Gaucher disease): Requires acidic environment for absorption.
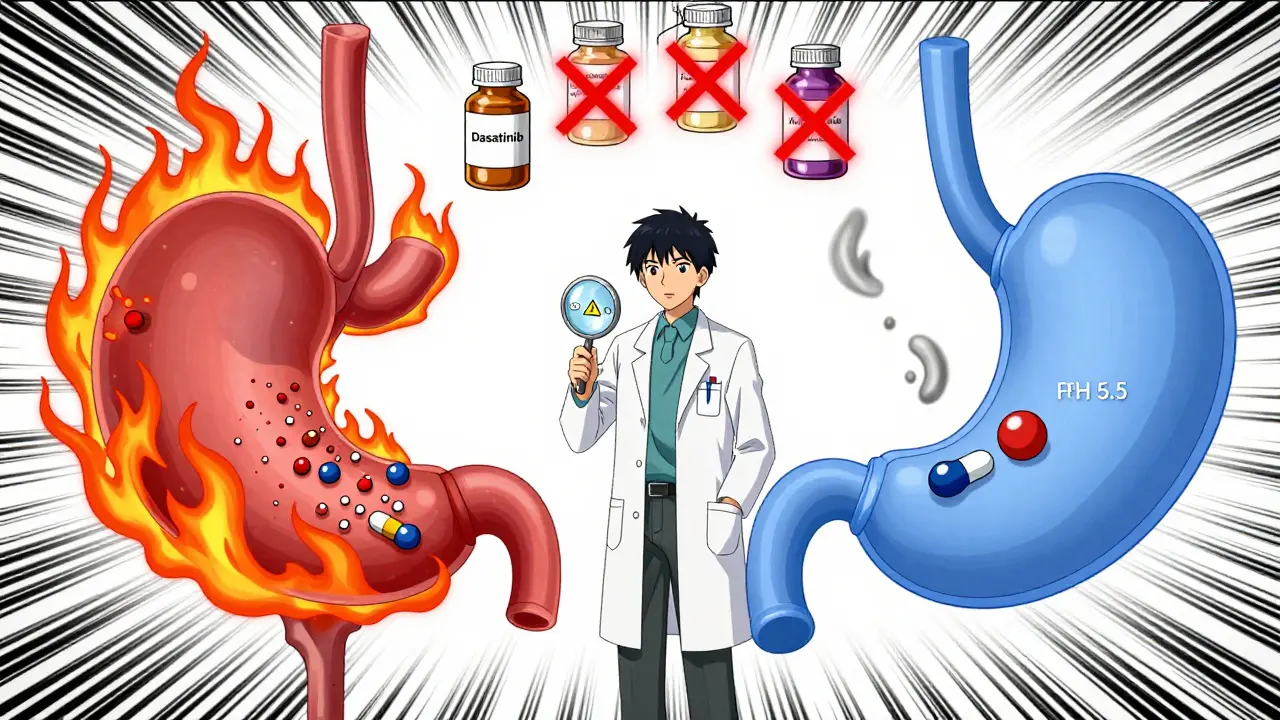
PPIs vs. H2 Blockers: Not All Are Equal
It’s tempting to think switching from a PPI to famotidine will solve the problem. It helps - but not enough. A 2024 study in JAMA Network Open found PPIs reduce absorption of pH-dependent drugs by 40-80%. H2 blockers? Only 20-40%. That’s still a big risk. Also, timing matters. Immediate-release pills are more vulnerable than extended-release versions. If you’re on dasatinib and take a PPI right after, the interaction is worse than if you take the PPI hours later. Even then, the effect isn’t fully avoided. Enteric-coated pills are another trap. These are designed to dissolve in the intestine, not the stomach. But if the stomach is too alkaline, they can dissolve too early - and get destroyed by acid before they’re absorbed. Or worse, they might not dissolve at all.Real-World Consequences
This isn’t theoretical. In a 2023 study of over 12,500 patients, those taking dasatinib with a PPI had 37% more treatment failures than those who didn’t. That means more relapses, more hospital visits, more cancer progression. On Reddit, users have shared stories of HIV treatment failing after starting Prilosec. One wrote: “My viral load went from undetectable to 12,000. My specialist said this is a classic interaction we test for in pharmacology.” Another user on Drugs.com said: “My doctor didn’t tell me Nexium would interfere with my blood pressure meds - my readings were consistently 20 points higher until we figured it out.” The FDA’s adverse event database recorded over 1,200 reports of therapeutic failure linked to acid-reducing drugs between 2020 and 2023. Atazanavir, dasatinib, and ketoconazole topped the list.What Can You Do?
If you’re on one of these high-risk drugs, don’t stop your acid reducer without talking to your doctor. But do ask these questions:- Is my medication affected by stomach acid?
- Can I switch to a different heartburn treatment?
- Can I take my drugs at different times?

Pharmacists Are Your Secret Weapon
Doctors are busy. They might not catch the interaction. But pharmacists? They’re trained to spot this. A 2023 study showed pharmacist-led reviews cut inappropriate ARA co-prescribing by 62% in Medicare patients. When you pick up a new prescription, ask your pharmacist: “Does this interact with my heartburn medicine?” Don’t assume they know what you’re taking. Bring a list - including over-the-counter pills and supplements. Many electronic health systems now flag dangerous combinations. Epic Systems reported 78% of doctors followed their alerts in 2023. But alerts aren’t perfect. You still need to speak up.The Future: Better Drugs, Smarter Systems
The pharmaceutical industry is waking up. Nearly 40% of new drugs in development now include pH-independent delivery systems - like special coatings or nanoparticles - to avoid this problem entirely. ClinicalTrials.gov lists 17 new candidates in Phase II or III trials designed to bypass acid sensitivity. AI tools are getting better too. Google Health’s 2024 prototype predicted ARA-drug interactions with 89% accuracy. In the next few years, your phone or EHR might warn you before you even fill the prescription. The FDA’s 2023 guidance now requires drugmakers to test new medications across pH levels 1.0-7.5. If a drug dissolves poorly above pH 5 and is a weak base, it gets flagged. That’s a big step forward.Bottom Line: Know Your Meds
Acid-reducing medications aren’t harmless. They’re powerful tools - but they change how your body handles other drugs. If you’re taking a pill for HIV, cancer, or a serious infection, your heartburn treatment could be sabotaging it. Ask your doctor or pharmacist: Is my medication affected by stomach acid? If you’re on a PPI long-term, ask if you still need it. You might be able to stop - or switch to something safer. This isn’t about avoiding acid reducers. It’s about using them wisely. When used correctly, they save lives. But when used without awareness, they can put lives at risk.Can I take omeprazole with my HIV medication?
No. Omeprazole and other PPIs can reduce the absorption of atazanavir by up to 95%, making it ineffective. This can cause HIV to rebound. If you need acid reduction, talk to your doctor about alternatives like antacids taken hours apart, or switch to an HIV drug that doesn’t interact, like raltegravir or dolutegravir.
Does famotidine (Pepcid) have the same interaction as omeprazole?
Famotidine has a lower risk than PPIs, but it still reduces absorption of drugs like dasatinib and ketoconazole by 20-40%. It’s not safe to assume it’s harmless. Always check with your pharmacist or doctor before combining any acid reducer with a critical medication.
How do I know if my drug is affected by stomach acid?
Look for drugs that are weak bases with low solubility at higher pH. Common signs: the drug’s label warns about acid reducers, it’s used for HIV, cancer, or fungal infections, or it’s taken on an empty stomach. Check the drug’s prescribing information for “drug interactions” or ask your pharmacist directly. Drugs with pKa above 7 are most likely to be affected.
Can I just take my pills at different times to avoid the interaction?
Spacing them out helps a little - taking the affected drug 2 hours before the acid reducer can reduce the interaction by 30-40%. But it doesn’t eliminate it. For high-risk drugs like atazanavir, timing doesn’t work. Avoidance is the only safe option.
Why don’t doctors always warn me about this?
Many doctors don’t realize how common and serious these interactions are. Acid reducers are seen as harmless, and patients rarely mention taking them unless asked. Studies show up to half of long-term PPI users have no medical reason for them. The problem is underrecognized - but awareness is growing. Don’t wait for your doctor to ask. Bring it up yourself.







Akshaya Gandra _ Student - EastCaryMS
January 4, 2026 AT 22:35i just started omeprazole last month for my acid and i take atazanavir too… wait no no no this cant be right???
Uzoamaka Nwankpa
January 6, 2026 AT 14:32My doctor never mentioned this. I’ve been on famotidine for 3 years with my leukemia meds. Guess I’m just lucky.
Oluwapelumi Yakubu
January 8, 2026 AT 01:53Let’s be real - modern medicine is a circus. We take pills to fix one thing, only to break ten others. The stomach isn’t just a chemical vat - it’s a sacred gatekeeper. When we meddle with pH like it’s a dial on a stereo, we’re not curing, we’re playing God with biochemistry. And don’t even get me started on how Big Pharma encourages this. PPIs are the aspirin of the 21st century: overprescribed, underunderstood, and dangerously normalized.
Enrique González
January 9, 2026 AT 13:40This is wild. I had no idea. I’ve been on omeprazole for years. Gonna ask my pharmacist tomorrow.
Aaron Mercado
January 9, 2026 AT 20:10Of course this is happening. The FDA doesn’t care. Doctors are too lazy. Pharmacies just fill prescriptions. You’re all just one pill away from a death sentence and nobody’s even blinking. I told my mom this exact thing last year - she ignored me. Now she’s in the hospital. Again.
John Wilmerding
January 11, 2026 AT 10:29This is an exceptionally well-documented and clinically significant interaction. The pharmacokinetic data is robust, particularly regarding weak base drugs with narrow therapeutic indices. The 2022 Celerion study on atazanavir demonstrates a statistically significant reduction in Cmax and AUC, with p-values <0.001. I strongly recommend all patients on high-risk medications undergo a comprehensive medication reconciliation with a clinical pharmacist. The American College of Gastroenterology’s 2022 deprescribing guidelines are also an essential reference. Proton pump inhibitors should be prescribed only for clear, evidence-based indications - not for occasional heartburn.
Peyton Feuer
January 12, 2026 AT 05:16my doctor just told me to "just take it at a different time" but i read this and now i’m scared. thanks for the heads up. gonna bring my meds list to the pharmacist this week.
Siobhan Goggin
January 12, 2026 AT 05:56So glad I found this. I’ve been on PPIs for years and just started a new cancer med. I’m scheduling a med review now. Knowledge is power!
Vikram Sujay
January 13, 2026 AT 19:03The human body operates on a delicate equilibrium of biochemical gradients. Stomach acidity is not a flaw to be corrected, but a physiological necessity evolved over millennia. To pharmacologically suppress it for non-life-threatening conditions is to mistake symptom management for healing. This is not merely a drug interaction - it is a systemic failure of medical education, corporate influence, and patient autonomy. We must return to the principle of minimal intervention. If the stomach is quiet, let it rest.
Jay Tejada
January 13, 2026 AT 20:10lol so my heartburn meds were secretly making my chemo useless? classic. guess i’ll be drinking apple cider vinegar now. jk. but seriously - why is this not on every prescription label? someone’s getting rich off this.
Shanna Sung
January 14, 2026 AT 17:38This is all a lie. The FDA is controlled by Big Pharma. They want you dependent on drugs. Acid-reducing meds are safe. Your body makes acid because you’re eating too much sugar. Go keto. Your pH will fix itself. They don’t want you to know this.
josh plum
January 15, 2026 AT 05:00People like you who take PPIs for "heartburn" are the reason healthcare is broken. You eat garbage, then pop a pill like it’s candy. Meanwhile, real patients with cancer are dying because you couldn’t be bothered to eat better. This isn’t a drug interaction - it’s karma. Stop being lazy and fix your diet. No one cares that you want to eat pizza at midnight.
John Ross
January 15, 2026 AT 09:02From a pharmacovigilance standpoint, this is a textbook case of a Class A drug-drug interaction - clinically significant, predictable, and preventable. The pharmacodynamic alteration of gastric pH directly impacts the ionization state of weak bases, thereby reducing passive diffusion across the gastric mucosa. The FDA’s 2023 guidance on pH-dependent solubility testing is a step forward, but real-world implementation remains inconsistent. Clinicians must integrate structured medication reconciliation protocols, and EHR systems must prioritize these interactions with hard stops, not soft alerts. This isn’t just clinical - it’s a systems failure.