When you hurt, you want relief. Fast. But not all pain meds are created equal-and the risks aren’t always obvious. For years, opioids were the go-to for serious pain. Now, doctors are changing their minds. Why? Because the data doesn’t lie: for most people, non-opioid options work just as well, with far fewer dangers.
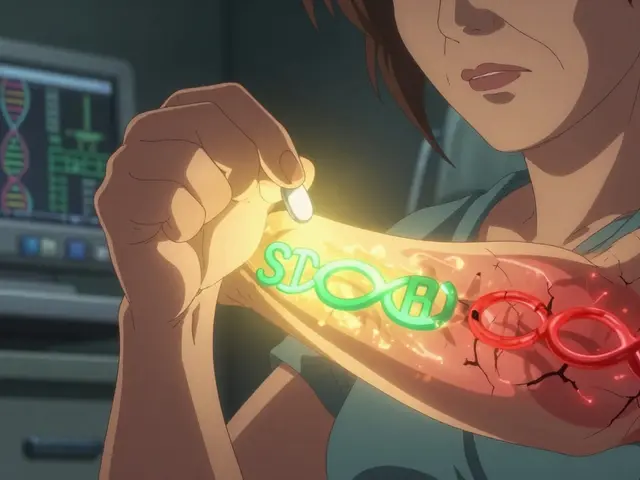
What Are Opioids, Really?
Opioids are drugs that bind to special receptors in your brain and spinal cord to block pain signals. They include morphine, oxycodone, hydrocodone, and fentanyl. Some come from the opium poppy; others are made in labs to mimic its effects. They’re powerful. And they’re addictive.
Back in the 1990s, pharmaceutical companies told doctors opioids were safe for long-term use. That turned out to be wrong. By 2017, the CDC called opioid overdoses a public health emergency. In 2021 alone, over 80,000 people in the U.S. died from opioid overdoses. That’s not just a statistic-it’s families losing parents, siblings, children.
Even if you don’t overdose, long-term use changes your body. A study of nearly 300,000 people found that taking opioids for more than 180 days over three years nearly tripled the risk of a heart attack. Daily doses above 120 mg of morphine equivalent doubled that risk. And that’s just one danger. Constipation, nausea, drowsiness, dependence-these aren’t side effects you can ignore. They’re part of the package.
Non-Opioids: The Quiet Alternative
Non-opioid pain relievers include everyday drugs like ibuprofen, naproxen, and acetaminophen. They work differently. Instead of targeting brain receptors, they reduce inflammation or block pain signals at the source. And they’ve been around for decades. Aspirin was invented in 1897. Acetaminophen came in the 1950s.
But here’s the surprise: for chronic pain-like back pain or arthritis-non-opioids often do just as well, if not better. A major 2018 study followed 240 patients with chronic back or joint pain for a full year. One group got opioids. The other got NSAIDs and acetaminophen. At the end of the year, both groups had similar levels of pain interference. But the non-opioid group had less pain intensity. They also had fewer side effects. No addiction. No risk of overdose.
And it’s not just adults. A 2024 review of five studies in children found no evidence that opioids like morphine or codeine worked better than ibuprofen for post-surgery or fracture pain. But the kids on opioids had way more nausea, vomiting, drowsiness, and even trouble breathing. Why risk that when ibuprofen works just as well?
The New Kid on the Block: Journavx
In March 2024, the FDA approved something new: Journavx. It’s the first new non-opioid painkiller class in decades. Unlike NSAIDs, it doesn’t irritate your stomach or raise blood pressure. Unlike opioids, it doesn’t slow your breathing or make you dependent.
It was tested on over 800 people after surgery-bunion removal, tummy tucks. Those who took Journavx had significantly less pain than those on placebo. And they didn’t need extra opioids for rescue pain relief. The FDA called it a major step forward in reducing opioid use. This isn’t a miracle drug, but it’s proof that safer alternatives are possible-and they’re being developed.

Why Doctors Are Changing Their Minds
The American College of Physicians, the CDC, the VA, and even state medical boards now say the same thing: start with non-opioids. For chronic pain, opioids shouldn’t be the first choice. They should be the last.
The CDC’s 2022 guideline says it plainly: use non-opioid therapy as the preferred treatment. If opioids are used at all, they should be paired with physical therapy, exercise, or other non-drug options. The VA’s own pain program says opioids weren’t superior to non-opioids in effectiveness-but came with far more side effects.
One doctor told me he used to prescribe oxycodone for lower back pain. Now, he starts with physical therapy, then acetaminophen, then naproxen. If that doesn’t work, he looks at nerve blocks or other targeted treatments. He doesn’t reach for opioids unless the patient has cancer or is in end-of-life care.
When Opioids Might Still Make Sense
Let’s be clear: opioids aren’t evil. They’re tools. And sometimes, the right tool for the job.
For cancer pain, severe trauma, or after major surgery, opioids can be lifesaving. But even then, the trend is shifting. Doctors now use them in short bursts-24 to 72 hours-alongside non-opioids. This is called multimodal pain control. It means hitting pain from multiple angles: one drug for inflammation, one for nerve pain, one for acute intensity. That way, you use less of each.
And not all opioids are the same. A 2023 study found that sustained-release oxycodone had a lower risk of overdose and death than sustained-release morphine in veterans. That means if opioids are needed, the choice matters. But again-this is for short-term, carefully monitored use. Not long-term.

What You Should Do If You’re on Opioids
If you’ve been on opioids for months or years, don’t stop cold turkey. Talk to your doctor. Ask these questions:
- Is this still helping me function better-or just masking pain?
- Have I had any side effects like constipation, dizziness, or mood changes?
- Am I taking more than I was a year ago?
- Have we tried non-opioid options like physical therapy, heat/cold, or NSAIDs?
Many people find they can reduce or stop opioids with the right support. A 2021 study showed that patients who switched to a non-opioid plan reported better sleep, more energy, and less anxiety-even if their pain didn’t disappear completely.
The Bottom Line
Pain is real. But the solution isn’t always a pill. For most people, non-opioid options are safer, just as effective, and come without the risk of addiction or overdose. The science is clear. The guidelines are clear. And now, new drugs like Journavx are making it easier than ever to manage pain without opioids.
You don’t have to suffer. But you also don’t have to risk your life for temporary relief. Start with what’s proven safe. Talk to your doctor. Ask for alternatives. Your body will thank you.
Are non-opioid painkillers as effective as opioids for chronic pain?
Yes, for most people with chronic pain like back pain or arthritis, non-opioid medications like NSAIDs and acetaminophen work just as well-or better-than opioids. A major 12-month study found no difference in pain-related function between the two groups, but the non-opioid group had lower pain intensity and fewer side effects. Opioids don’t improve long-term function, and they carry serious risks.
Can you get addicted to opioids even if you take them as prescribed?
Yes. Addiction isn’t about how you take the drug-it’s about how your brain responds. Even when taken exactly as directed, opioids change brain chemistry over time. Studies show that after just five days, the risk of long-term use increases. After 30 days, dependence becomes common. That’s why doctors now avoid prescribing them for more than a few days unless it’s for cancer or end-of-life care.
What are the biggest risks of long-term opioid use?
The biggest risks are addiction, overdose, and heart problems. Long-term opioid use increases your chance of heart attack by nearly 2.7 times. It also causes constipation, hormonal changes, depression, and sleep apnea. Even if you don’t overdose, your body becomes dependent. Stopping suddenly can cause severe withdrawal. These risks outweigh the benefits for most chronic pain conditions.
Is Journavx better than ibuprofen or acetaminophen?
Journavx isn’t meant to replace ibuprofen or acetaminophen. It’s a new type of non-opioid painkiller designed for short-term acute pain-like after surgery. It works differently than NSAIDs, so it doesn’t irritate the stomach or affect blood pressure. For everyday pain, ibuprofen or acetaminophen are still first-line. For post-surgery pain, Journavx offers a safer alternative to opioids, not necessarily a replacement for NSAIDs.
Can children safely take opioids for pain after surgery?
No, not routinely. A 2024 review of five studies found no evidence that opioids like morphine or codeine work better than ibuprofen for children after surgery or fractures. But children on opioids had far more side effects: nausea, vomiting, drowsiness, and even low oxygen levels. For kids, non-opioid pain relief is safer and just as effective.
What should I do if my doctor still prescribes opioids for chronic pain?
Ask why. Request a plan to try non-opioid options first-like physical therapy, exercise, or NSAIDs. Bring up the CDC’s 2022 guidelines, which say non-opioids should be the first treatment. If your doctor refuses to consider alternatives, it may be time to seek a second opinion from a pain specialist who follows current evidence-based practices.







Jefriady Dahri
November 25, 2025 AT 08:05Just wanted to say this post hit home for me. My dad was on opioids for years after a back injury and it nearly broke our family. He didn’t OD, but he became a shadow of himself-sleepy, withdrawn, always constipated. When we switched him to naproxen and physical therapy? He started laughing again. Took time, but it was worth it. You don’t need a miracle drug to feel human again.
Roscoe Howard
November 26, 2025 AT 12:44It is imperative to note that the systemic erosion of pharmaceutical oversight in the United States has led to an unprecedented public health catastrophe. The CDC’s 2022 guidelines are not merely recommendations-they are evidence-based imperatives. The normalization of opioid prescriptions as a first-line intervention constitutes a profound failure of medical ethics and regulatory governance. Furthermore, the FDA’s approval of Journavx, while commendable, remains a reactionary measure rather than a proactive paradigm shift.
Kimberley Chronicle
November 28, 2025 AT 11:24Really appreciate this breakdown-it’s refreshing to see such a nuanced take on pain management. The multimodal approach is where the real innovation lies. Journavx is a game-changer for acute post-op contexts, but let’s not overlook the foundational role of NSAIDs and acetaminophen. They’re low-cost, well-studied, and accessible. The key is stratification: match the drug to the pathology, not the patient’s anxiety. Also, physical therapy isn’t just adjunct-it’s core. We need to reframe pain as a biopsychosocial phenomenon, not a biochemical deficit.
giselle kate
November 30, 2025 AT 02:04They want you to believe non-opioids are ‘just as good’ because they’re trying to cover up the fact that Big Pharma and the government are colluding to kill off the opioid industry after they made their billions. They don’t want you to know that opioids still work better for real pain-like cancer or nerve damage. But they’ll force you onto ibuprofen until you’re screaming in agony because it’s cheaper and they don’t care about your suffering. This is control. They don’t want you to feel too good. They want you docile. And now they’re pushing this Journavx nonsense like it’s the holy grail. It’s not. It’s a Trojan horse.
Emily Craig
December 1, 2025 AT 02:12So let me get this straight… we spent 20 years telling people opioids were safe, then suddenly everyone’s a pain specialist overnight? 🙄
My cousin’s mom took oxycodone for 7 years after a car crash. She didn’t OD. She didn’t become a zombie. She just… stopped living. Now she hikes, paints, and laughs without needing a prescription. So yeah. Non-opioids won. And guess what? The sky didn’t fall. Your pain didn’t vanish-but your life got better. That’s the real win.
Archana Jha
December 1, 2025 AT 10:04you know what no one talks about? the fact that the fda approved journavx right after the big pharma execs all went on vacation? coincidence? i think not. also why are there no long term studies? they just threw it at us like its a magic bullet. and dont get me started on the va and cdc theyre all part of the same system that let oxycontin get approved in the first place. i dont trust any of this. also i think the government is using pain meds to control the population. its not about health its about power
Aki Jones
December 2, 2025 AT 09:45It’s not merely that opioids are dangerous-it’s that their long-term use induces neuroadaptive changes that fundamentally alter reward processing, emotional regulation, and autonomic function. The 2.7x increase in myocardial infarction risk is not statistically insignificant; it is a clinical catastrophe. Furthermore, the normalization of ‘tolerance’ as a benign phenomenon ignores the pharmacokinetic cascade that leads to respiratory depression, hypogonadism, and opioid-induced hyperalgesia. Journavx, while novel, lacks longitudinal data beyond 90 days. We are trading one unknown for another. And yet, the public discourse remains dangerously reductive: ‘ibuprofen = good, opioids = evil.’ Reality is far more complex.
Rachel Villegas
December 4, 2025 AT 03:18My mom switched from oxycodone to gabapentin and naproxen after 12 years. She went from barely getting out of bed to gardening every morning. No one told her she could do that. She didn’t need to be ‘stronger’-she just needed better options. This isn’t about willpower. It’s about medicine catching up to science. Thank you for writing this.