Going out to eat shouldn’t mean giving up control over your blood sugar. With diabetes, dining at a restaurant can feel like walking through a minefield-sauces loaded with sugar, oversized portions, and hidden carbs hiding in plain sight. But it doesn’t have to be that way. Thousands of people with diabetes eat out regularly without spiking their glucose, and the secret isn’t avoiding restaurants. It’s knowing what to look for, how to ask for what you need, and how to adjust your plate before the food even arrives.
Use the Plate Method-No Math Required
You don’t need a calculator or an app to eat well at a restaurant. The Diabetes Plate Method works because it’s visual, simple, and works across every cuisine. Grab a nine-inch plate (the size most restaurants serve on) and divide it in your mind: half the plate gets filled with non-starchy vegetables. That means broccoli, spinach, green beans, zucchini, peppers, or salad greens. These add volume, fiber, and nutrients without pushing your blood sugar up. A quarter of the plate is for lean protein-grilled chicken, fish, tofu, or lean beef. Stick to about the size of your palm, which is roughly 3 to 4 ounces. The last quarter? That’s your carb zone. And here’s the catch: that quarter shouldn’t be a mountain of rice, pasta, or mashed potatoes. It should be about the size of your fist-or less.Portion Sizes in Restaurants Are Not Normal
Think about the last time you ate out. How big was that plate of pasta? Or the basket of bread? Most restaurant portions are two to three times larger than what’s recommended for someone managing diabetes. A typical serving of rice at home is half a cup. At a restaurant? It’s often a full cup or more-that’s 45 grams of carbs right there, just from the side. The same goes for pasta, potatoes, and even quinoa. Your best move? Ask for a half portion of starchy sides. Or better yet, swap them out. Instead of fries, ask for extra steamed vegetables. Instead of mashed potatoes, go for a side salad with vinaigrette. Most places will do it without making a fuss.Watch Out for Hidden Carbs
The biggest trap isn’t what you see-it’s what you don’t. Sauces, glazes, dressings, and gravies are carb bombs. Teriyaki sauce? 10 grams of sugar per tablespoon. Creamy pasta sauce? Often loaded with flour or cornstarch. Even "healthy" options like hummus or tomato soup can hide 15 grams of carbs in a small serving. Always ask for sauces and dressings on the side. That way, you control how much you use. Two tablespoons max. And if you’re unsure, skip it. A plain grilled chicken breast with vegetables is safer than anything smothered in sauce.Know the Red Flag Words on Menus
Certain words should send up a red flag. "Crispy," "breaded," "creamed," "au gratin," "stuffed," and "croutons" all mean extra carbs. A "crispy chicken sandwich" isn’t just fried-it’s coated in flour, then breaded, then fried again. That’s easily 50 grams of carbs before you even add the bun. Instead, look for words like "grilled," "baked," "steamed," or "roasted." These usually mean less processing and fewer hidden carbs. If you’re ordering Asian food, avoid anything labeled "sweet and sour," "honey garlic," or "orange chicken." Those sauces are pure sugar. Go for steamed dishes with ginger and soy sauce on the side.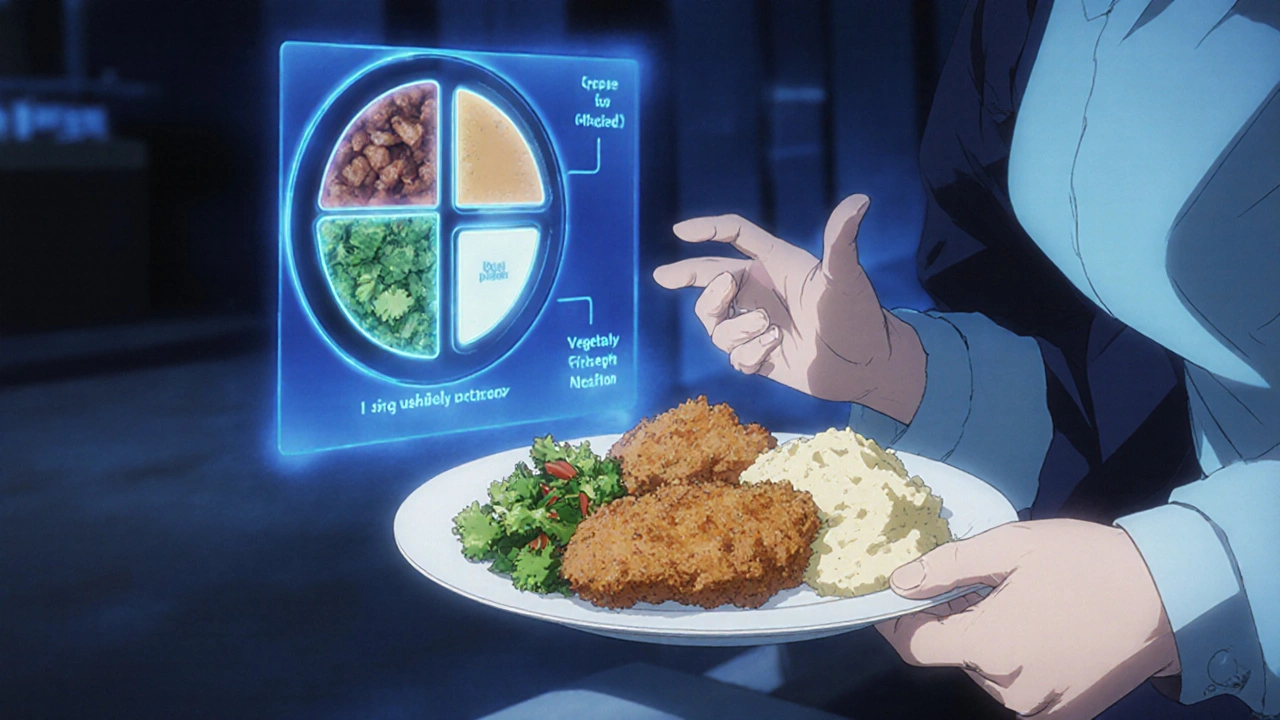
Plan Ahead-Don’t Wing It
One of the biggest mistakes people make? Showing up hungry and ordering the first thing that sounds good. That’s when you end up with a giant pizza or a loaded burrito. Instead, check the menu online before you leave the house. Most chains now have nutrition info posted. Look for meals with 45 grams of carbs or less-that’s the sweet spot for most adults with diabetes. If the restaurant doesn’t list carbs, use the plate method as your guide. And if you’re going to a new place, pick two or three options ahead of time. That way, when you get there, you’re not guessing. Studies show people who plan ahead are 42% more likely to stick to their carb goals.Share, Split, or Pack It Up
Restaurant portions are designed to overwhelm. You don’t have to eat it all. Share your main dish with someone else. Order an appetizer-sized portion if it’s available. Or, as soon as your food comes, ask for a to-go box and pack up half before you even take a bite. This simple trick cuts your carb intake in half without anyone noticing. It also gives you a ready-made lunch for the next day. No need to cook. No need to stress.Don’t Skip Meals or Go Too Hungry
Going to a restaurant starving is a recipe for disaster. When you’re ravenous, your brain goes straight for the carbs. You grab the bread basket, order the pasta, and down the soda because you’re so hungry you can’t think straight. Instead, eat a small snack before you leave-like a handful of nuts, a hard-boiled egg, or a slice of cheese. That takes the edge off your hunger so you can make smarter choices when you get there. Research shows this cuts high-carb choices by 37%.Carry Glucose Tablets Just in Case
Restaurants aren’t always fast. If you’re on insulin, waiting 45 minutes for your food can send your blood sugar dropping. Always carry fast-acting glucose-like tablets or juice-in your bag. Keep at least 15 grams on hand. If you start feeling shaky, dizzy, or sweaty, take one. Better safe than sorry. About 23% of people with diabetes report having a low blood sugar episode while dining out. You don’t want to be one of them.
Ask for Help-It’s Okay
You might feel awkward asking for substitutions or extra veggies. But here’s the truth: most servers have heard it before. Many restaurants now train staff on dietary needs. And if they don’t know the answer, they’ll ask the chef. Don’t be afraid to say: "I have diabetes and need to keep my carbs low. Can I get the chicken without the sauce, and swap the fries for steamed broccoli?" You’re not being difficult. You’re taking care of your health. And honestly? Most people are impressed when someone knows what they need and asks clearly.Technology Can Help-But Don’t Rely on It
Apps like the American Diabetes Association’s "Restaurant Ready" can give you carb counts for over 15,000 menu items. That’s useful. But don’t trust every number you see. A 2023 study found only 32% of restaurant carb labels are accurate. Use apps as a guide, not a gospel. Always double-check with the plate method. And if you have a continuous glucose monitor (CGM), use it. Seeing your blood sugar rise after a meal tells you more than any app ever could.It’s Not Perfect-But It’s Possible
Some days, you’ll eat something that spikes your sugar. That’s okay. What matters is what you do next. Don’t beat yourself up. Learn from it. Did the sauce have more sugar than you thought? Next time, ask for it on the side. Did the portion come out huge? Pack half away before you start. Progress isn’t about being perfect. It’s about making better choices most of the time. People who stick to these habits for six months often see their HbA1c drop by 0.8% to 1.2%. That’s not magic. That’s smart choices.Can I still eat pasta when I have diabetes?
Yes-but in small amounts. Stick to half a cup of whole grain or legume-based pasta, and pair it with a large portion of vegetables and lean protein. Avoid creamy sauces and opt for tomato-based or olive oil-based options. Always check the carb count on the package and adjust your insulin if needed.
Are salads always a safe choice?
Not always. A salad with croutons, cheese, bacon, and creamy dressing can have more carbs than a burger. Stick to leafy greens, grilled chicken or shrimp, and ask for vinaigrette on the side. Use no more than two tablespoons. Skip the candied nuts and dried fruit-they’re sugar bombs.
What’s the best fast food option for someone with diabetes?
Grilled chicken salad (without croutons or sugary dressing), a plain grilled chicken sandwich without the bun, or a taco salad with beans and veggies are good picks. Avoid fried items, burritos, and wraps. McDonald’s grilled chicken salad has about 18 grams of carbs-much better than a Big Mac at 46 grams.
Should I avoid alcohol when eating out?
You don’t have to avoid it, but be careful. Beer and sweet cocktails can spike your blood sugar. Dry wine, light beer, or spirits with soda water and lime are better choices. Always drink with food, and check your blood sugar before bed if you drink. Alcohol can cause delayed lows, especially if you’re on insulin or certain pills.
How do I handle social pressure to eat more?
Say it plainly: "I’m managing my diabetes, so I need to keep portions small." Most people understand once you explain. If someone offers you a bite, say yes-but take just a taste. You don’t have to finish everything on your plate. Your health comes first, and real friends will respect that.
What if the restaurant doesn’t have healthy options?
Even at steak houses or burger joints, you can usually find something. Order a grilled steak or chicken, ask for a side of vegetables instead of fries, and skip the bread. If there’s no veggie option, ask if they can steam or sauté some spinach or broccoli. Most kitchens can do it. If they can’t, bring a snack from home to balance your meal.







mike tallent
November 17, 2025 AT 11:34Love this post! 🙌 The plate method is my go-to when I’m out with friends. I just mentally divide my plate and ask for extra veggies - no one even notices. I’ve lost 12 lbs in 6 months just by doing this. Also, carrying glucose tabs? Game changer. Been there, done that, got the t-shirt (and the emergency glucose). 💪
Peter Stephen .O
November 17, 2025 AT 21:56Same here. I used to avoid restaurants until I learned to ask for sauces on the side. Now I hit up sushi places all the time - just grab sashimi, edamame, and miso soup. No rice, no soy sauce unless it’s a splash. My A1c dropped from 8.2 to 6.7 in 5 months. You don’t need to be perfect, just consistent. And yes, the plate method works even at taco joints 🌮
Julie Roe
November 19, 2025 AT 12:14As someone who’s been living with type 2 for 14 years, I can tell you this: the real win isn’t the plate method - it’s the mindset shift. You stop seeing food as forbidden and start seeing it as fuel. I used to feel guilty eating out. Now I plan. I check menus. I pack a snack. I ask for substitutions like it’s my job. And guess what? My family thinks I’m weird now, but they’ve started doing it too. My 16-year-old daughter just asked the waiter for grilled chicken without the glaze. She’s 16. She knows her body. That’s the real victory. You’re not just managing diabetes - you’re modeling health for everyone around you. Keep going. 🌱
Deepali Singh
November 19, 2025 AT 21:10So you’re telling me I can’t have that butter chicken curry anymore? 😏 I mean, I know it’s 70g of carbs, but the sauce? The aroma? The *texture*? I’d rather have a low A1c and a sad soul. Just saying.
Joyce Genon
November 20, 2025 AT 22:24Let’s be real - this whole ‘plate method’ is just a fancy way of saying ‘eat less.’ And don’t get me started on the ‘nutrition info’ on menus. I’ve seen restaurants list ‘15g carbs’ for a pasta dish that clearly had 40g. The FDA doesn’t even regulate this stuff. And who the hell has time to check every menu online before dinner? I work 60 hours a week. I’m tired. I just want to eat. This post feels like a guilt trip wrapped in a wellness influencer’s Instagram filter.
John Wayne
November 21, 2025 AT 15:03Interesting. But you’re assuming everyone has access to grilled chicken, steamed broccoli, and servers who care. What about rural towns? What about fast food chains in food deserts? Or people on fixed incomes? This reads like a luxury guide for people who can afford to ‘swap’ sides. Real people eat what’s cheap, fast, and available. Your advice is nice. But it’s not universal.
Jennifer Howard
November 22, 2025 AT 15:48While I appreciate the sentiment, I must point out that the claim regarding ‘42% more likely to stick to carb goals’ is statistically dubious without a cited peer-reviewed source. Furthermore, the reference to ‘23% of people with diabetes report low blood sugar episodes while dining out’ is anecdotally derived and lacks temporal or geographic context. The use of emoticons and colloquialisms undermines the scientific rigor expected in medical guidance. I recommend consulting the American Diabetes Association’s 2024 Standards of Care, which, unlike this post, are evidence-based and peer-reviewed.
Sylvia Clarke
November 23, 2025 AT 23:18Oh, honey. You’re telling me I can’t have that creamy mushroom risotto at the Italian place I’ve been dying to try since 2019? 😭 I’m not asking for a miracle - I’m asking for a little joy. Maybe we don’t need to ‘control’ every bite. Maybe we just need to enjoy the damn food and adjust the insulin. I’ve been doing this for 17 years. I’ve had highs. I’ve had lows. I’ve cried over bread baskets. But I’ve also laughed with friends over tiramisu. Life isn’t a spreadsheet. Sometimes, the carbs are worth it. And if you’re on insulin? You’ve got the tools. Use them. Don’t fear the food. Fear the shame.
Andrew Cairney
November 25, 2025 AT 04:12Wait… so you’re telling me restaurants are hiding carbs in sauces? DUH. That’s why I don’t trust ANYTHING. The government, the FDA, the restaurants - they’re all in cahoots. They want us fat. They want us diabetic. That’s why they put ‘healthy’ on the menu. It’s a trap. I only eat meat I kill myself. And I don’t go out. Ever. I cook in my bunker. With solar-powered pans. And I only use sea salt from the Andes. 🤫
vinod mali
November 26, 2025 AT 04:06Bro this is gold. I’m from Delhi, and we eat out all the time - parathas, biryani, dosas. But I just ask for less rice, extra sabzi, and skip the chutney. No big deal. People think I’m weird but they copy me now. My cousin even started using a small plate at home. Simple stuff works. No apps needed. Just eat smart. 🙏
Rob Goldstein
November 26, 2025 AT 06:50One thing missing here: insulin timing. If you're on rapid-acting insulin, carb counting alone isn't enough - you need to consider the glycemic load and absorption kinetics. A bowl of brown rice has a lower GI than white rice, but if it's served with a high-fat curry, the carb absorption is delayed. That means you might need to split your bolus or use an extended wave. Always correlate your insulin timing with your meal composition. CGM data is your best friend here - look for the shape of the curve, not just the peak.
Gary Lam
November 27, 2025 AT 14:09As a Thai guy who runs a noodle shop - I get it. You want to eat pad thai? Fine. But I’ll give you half the noodles, double the veggies, and no sugar in the sauce. No one ever says no. And I’ve seen diabetic customers come back every week. You just gotta ask. And if they say no? Find a better place. Life’s too short for bad service AND bad carbs.
jalyssa chea
November 29, 2025 AT 08:04why even bother with restaurants at all if you have diabetes just eat home cooked food its 2024 why are you still going out i mean seriously
Abdul Mubeen
November 30, 2025 AT 15:57It’s curious how this article assumes that all individuals with diabetes have the same metabolic responses, the same access to healthcare, and the same level of health literacy. It ignores socioeconomic disparities, the psychological burden of constant self-monitoring, and the fact that many patients are prescribed insulin without adequate education. This is not empowerment - it’s victim-blaming disguised as advice. Who wrote this? A dietitian? Or a marketing consultant for a glucose monitor company?