PAMORA Selection Tool
PAMORA Selection Tool
This tool helps determine which peripherally acting mu-opioid receptor antagonist (PAMORA) may be most appropriate for managing opioid-induced constipation based on your individual health circumstances.
Recommended PAMORA
When you’re on long-term opioids for pain, constipation isn’t just an inconvenience-it can make you stop taking your medicine altogether. Up to 80% of people using opioids for chronic pain develop opioid-induced constipation (OIC), and traditional laxatives often don’t cut it. Studies show less than 30% of patients get consistent relief from stool softeners or fiber supplements. That’s where peripherally acting mu-opioid receptor antagonists (PAMORAs) come in. These drugs don’t touch your pain relief but fix the gut problems opioids cause.
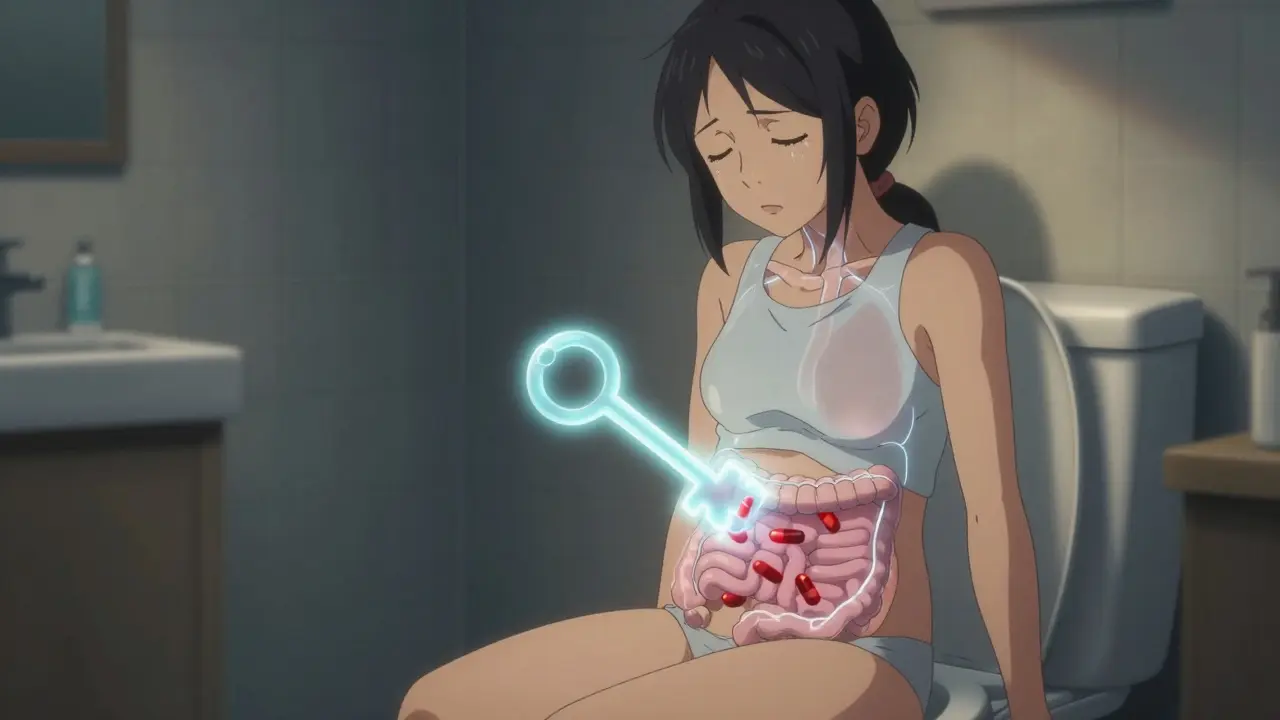
Why Opioids Cause Constipation
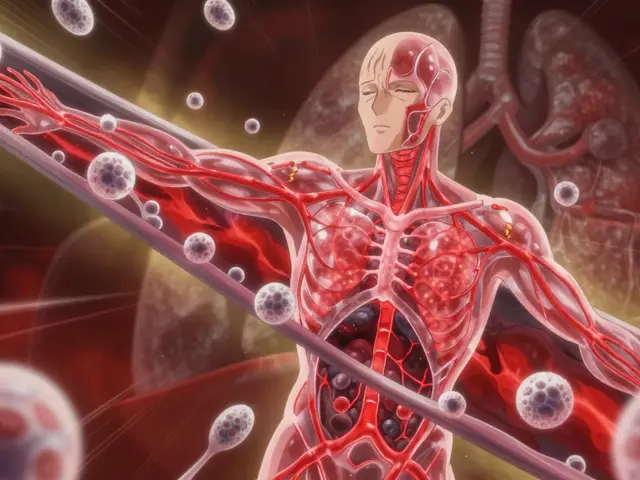
Opioids don’t just work in your brain. They bind tightly to mu-opioid receptors all over your body, especially in your intestines. These receptors control how fast food moves through your gut, how much fluid gets absorbed, and how your muscles contract. When opioids lock onto them, your bowel slows down. Stools get hard, you feel bloated, and you might go days without a bowel movement. It’s not laziness or diet-it’s biology. And unlike regular constipation, this one doesn’t respond well to lifestyle changes alone.How PAMORAs Work
PAMORAs are designed to block opioid receptors only in the gut. They’re built to stay out of the brain, so they don’t interfere with pain control. Think of them like targeted keys that unlock only the gut’s opioid receptors, not the brain’s. Three main drugs make up this class: methylnaltrexone, naloxegol, and naldemedine. Each has a slightly different chemical structure, but they all do the same thing: restore normal bowel movement without dulling your pain relief.The Three Main PAMORAs
- Methylnaltrexone (RELISTOR): Available as a shot or pill. It’s the only one approved for both cancer and noncancer pain patients. It works fast-half of users have a bowel movement within 4 hours. It doesn’t get broken down by liver enzymes, so it plays nice with other meds. Dose is based on weight for injections, and 450 mg daily for pills.
- Naloxegol (MOVANTIK): An oral tablet taken once daily. It’s a modified version of naloxone with a polyethylene glycol chain to keep it out of the brain. Works best when taken 1 hour before your opioid dose. Not recommended if you have severe kidney problems.
- Naldemedine (SYMPROIC): Also oral, taken once a day. It’s built with a similar peripheral-restriction design. Clinical trials showed nearly half of patients had regular bowel movements without increasing pain. Safe for most kidney patients, but avoid if you have a bowel blockage.
All three are contraindicated if you have a mechanical obstruction in your gut. That’s non-negotiable. Taking them in that case could lead to dangerous pressure buildup or even rupture.

How Effective Are They?
Clinical data speaks clearly. In trials with over 1,000 patients, methylnaltrexone led to bowel movements in 52% of users within 4 hours-compared to just 30% on placebo. Naloxegol helped 44% of patients have spontaneous bowel movements over 12 weeks. Naldemedine hit 48%, beating placebo by over 13 percentage points. These aren’t minor improvements. For many, it’s the difference between being stuck at home and being able to leave the house.Real-world feedback is mixed but telling. On patient forums, cancer patients report life-changing results with methylnaltrexone. One Reddit user wrote, “I hadn’t had a real bowel movement in 10 days. After the first shot, I went within 3 hours. I cried.” Meanwhile, people on long-term pain meds for arthritis or back issues say naloxegol worked for a while, then stopped. Cost is a huge issue-$5,000 to $6,000 a year without insurance. Many rely on manufacturer coupons just to afford it.
When and How to Take Them
Timing matters. PAMORAs work best when taken about an hour before your opioid reaches its peak effect. If you take oxycodone at 8 a.m. and 8 p.m., take your PAMORA at 7 a.m. and 7 p.m. This keeps the gut receptors blocked right when the opioid is most active in your intestines.Methylnaltrexone injections need to be administered by a nurse at first, especially for cancer patients. After that, many can self-inject. Pills are easier-just swallow them daily. But don’t skip doses. Consistency is key. If you miss one, take it as soon as you remember-but not if it’s close to your next dose.
Side Effects and Risks
Most side effects are mild: stomach cramps, nausea, diarrhea, or sweating. About 1 in 3 people report abdominal pain, especially at the start. That usually fades after a week. But here’s the catch: if you have severe kidney disease, naloxegol is off-limits. Methylnaltrexone needs a dose cut in half if your kidneys are failing. Naldemedine is safest for kidney patients.Alvimopan, another PAMORA, is only used in hospitals after bowel surgery because of heart risks. It’s not for long-term pain patients. The FDA requires a special program to track its use due to rare but serious heart attacks seen in trials.
Cost and Access
These drugs are expensive. In 2022, methylnaltrexone made $1.26 billion in sales. Naloxegol brought in $840 million. But most patients don’t pay full price. Manufacturer programs offer copay cards that reduce monthly costs to under $50. Without them, many just give up. A 67-year-old woman on Healthgrades said, “I used it for two weeks, then it stopped working. I paid $450 a month for nothing.” That’s the reality for many.Insurance coverage varies. Some require trying laxatives first. Others only cover it for cancer patients. The American Gastroenterological Association warns that without price cuts, only 35-40% of eligible patients will ever get access.
What’s Next?
New developments are coming. In January 2023, a new 300 mg tablet of methylnaltrexone got approved for patients who didn’t respond to the standard dose. Researchers are testing a combo drug that blocks opioid receptors in the gut while also stimulating gut movement with a serotonin agonist. Early results show 68% response rates-better than any single drug so far.Biosimilars are on the horizon. A Chinese company is in phase 3 trials for a methylnaltrexone copy. If it gets approved in the U.S., prices could drop significantly. But until then, PAMORAs remain the only treatment that targets the actual cause of opioid constipation-not just the symptoms.
Bottom Line
If you’re on opioids and stuck with constipation, don’t accept it as normal. PAMORAs are the first class of drugs designed to fix the root problem. They’re not perfect-they’re pricey, can cause cramps, and require careful timing. But for many, they’re the only thing that lets them keep their pain medication without sacrificing their quality of life. Talk to your doctor about whether one of these drugs is right for you. If cost is an issue, ask about patient assistance programs. You don’t have to suffer in silence.Can PAMORAs reduce my pain relief?
No. PAMORAs are designed to stay out of the brain and only block opioid receptors in the gut. Multiple clinical trials confirm they don’t interfere with pain control. In fact, patients often report better pain management because they can stick to their full opioid dose without being sidelined by constipation.
How long does it take for PAMORAs to work?
It varies by drug. Methylnaltrexone injections work in as little as 30 minutes, with most people having a bowel movement within 4 hours. Oral forms like naloxegol and naldemedine take longer-usually 12 to 24 hours for the first effect. Regular use leads to more predictable bowel movements after a few days.
Are PAMORAs safe for elderly patients?
Yes, but with caution. Older adults are more sensitive to side effects like cramping and diarrhea. Dosing may need adjustment, especially if kidney function is reduced. Methylnaltrexone is often preferred in this group because it’s available as an injection, allowing precise dosing. Always monitor for dehydration or electrolyte imbalance.
Can I use PAMORAs with other laxatives?
You can, but it’s usually unnecessary. PAMORAs are more effective than traditional laxatives for opioid-induced constipation. If you’re still not having regular bowel movements after 2-3 weeks on a PAMORA, your doctor may add a mild osmotic laxative like polyethylene glycol. Avoid stimulant laxatives long-term-they can damage the colon.
Why is alvimopan not used for chronic pain?
Alvimopan was linked to increased risk of heart attack in long-term use during clinical trials. Because of this, it’s only approved for short-term use (up to 7 days) after bowel surgery in hospital settings. It’s not approved for chronic opioid users due to safety concerns.
Is there a generic version of PAMORAs?
Not yet. All three main PAMORAs-methylnaltrexone, naloxegol, and naldemedine-are still under patent protection. The first biosimilar for methylnaltrexone is in phase 3 trials in China and may reach the U.S. market by 2027. Until then, patient assistance programs are your best bet for affordability.





Kelly Weinhold
January 31, 2026 AT 02:35Okay, I just want to say thank you for writing this. I’ve been on oxycodone for 7 years for my back, and I was starting to think I was just weak or lazy for not being able to poop regularly. Turns out? My gut was just hijacked. I started on methylnaltrexone after my GI doc basically yelled at me to stop relying on Miralax like it’s candy. First shot? I was in the bathroom within 2 hours. I cried. Not because it hurt-because I finally felt like myself again. If you’re suffering and think it’s normal? It’s not. Talk to your doctor. You deserve to move without shame.
Also, the cost is insane, but the copay card from the manufacturer cut my bill from $500 to $45. I know it’s not perfect, but it’s life-changing. Don’t give up.
And yes, I still take my laxatives on off-days. But now I’m not trapped in my house for a week. That’s worth every penny.
Also, I self-inject now. It’s not as scary as it sounds. Nurse taught me, and now I do it while watching Netflix. No big deal.
Also also, my dog started licking my face every time I take the shot. He knows what’s coming. He’s my little bowel movement cheerleader.
Also also also-please don’t let anyone tell you it’s ‘just constipation.’ This is a medical issue. Period.
Also also also also-I’m gonna start a support group. Anyone wanna join? We’ll call it ‘Poop Liberation Front.’ I’ve got merch ideas already.
Also also also also also-I’m not sorry for being long-winded. This matters.
Also also also also also also-I’m so glad I found this thread. I didn’t think anyone else got it.
Also also also also also also also-I’m gonna go poop right now. And I’m gonna enjoy it.
Also also also also also also also also-I love you all. Stay well.
Sheila Garfield
February 1, 2026 AT 04:39My mum’s on naldemedine and it’s been a game-changer. She’s 78, has arthritis, and was basically constipated for 18 months straight. Started it in January and now she’s going daily without cramps. No more panic when she leaves the house. She even went on a cruise last month. Didn’t bring a single laxative. Just her pills and a tiny bottle of water. She’s proud. So am I.
Cost was a nightmare at first, but the manufacturer’s program covered 80%. Took three calls and a fax, but worth it. Don’t let the price scare you off.
Shawn Peck
February 2, 2026 AT 06:41Y’all are overcomplicating this. It’s just constipation. Take a laxative. Done. Why are you paying $5k a year for a fancy pill that just makes you cramp? My uncle took this stuff and still pooped once a week. You’re wasting money. Just eat prunes. Or better yet-stop taking opioids. You don’t need them. Pain is a mindset. I fixed mine with yoga and affirmations.
Niamh Trihy
February 2, 2026 AT 07:55Shawn, I get where you’re coming from-but this isn’t about willpower. Opioid-induced constipation is a pharmacological blockade in the gut, not a dietary issue. Laxatives don’t touch the mechanism. PAMORAs do. It’s like trying to fix a broken fuel line by shaking the gas tank. You can shake all day, but the car still won’t start.
And no, prunes won’t help if your gut’s frozen by mu-receptor binding. This is biology, not a lifestyle hack.
Also, if your uncle still pooped once a week after using it? He might’ve been on too low a dose. Or had an obstruction. That’s why you need a doctor’s guidance.
And yes, the cost sucks. But that’s a system failure, not a treatment failure. Let’s not punish patients for corporate greed.
Sarah Blevins
February 3, 2026 AT 01:20The data presented here is methodologically flawed. The clinical trials cited have small sample sizes, lack long-term follow-up, and conflate spontaneous bowel movements with functional improvement. Additionally, patient testimonials are anecdotal and subject to confirmation bias. The assertion that PAMORAs are ‘the only treatment targeting the root cause’ ignores the role of multimodal interventions-hydration, mobility, dietary fiber, and biofeedback-which are underutilized and under-researched in this context.
Furthermore, the cost-benefit analysis is omitted. At $5,000 annually per patient, with only 45% response rates, this represents poor value for healthcare systems. The FDA’s approval does not equate to clinical superiority.
Recommendation: Re-evaluate treatment algorithms before endorsing high-cost pharmacotherapy as first-line.
Jason Xin
February 3, 2026 AT 03:59Wow. So we’ve got a whole TED Talk on how to poop while on opioids. Meanwhile, the guy who invented this drug is probably on a yacht in the Caymans, laughing while his stock ticker goes up.
But hey-kudos to the people who actually got relief. That’s real. And yeah, the price is a scam. But let’s not pretend this isn’t Big Pharma’s latest ‘fix’ for a problem they helped create.
Still… if it works, it works. I’d rather pay $5k to not be stuck on the toilet for 10 days than take another laxative that just makes me feel like a balloon. So… I’m not mad. Just… tired.
Gaurav Meena
February 4, 2026 AT 00:18As someone from India, I’ve seen patients here struggle with this too-but they can’t even get access to the basics. My cousin’s dad is on morphine for cancer pain, and they’re using castor oil and enemas because PAMORAs are 10x more expensive here. I’m so glad this info is out there. Maybe someday, generics will reach places like ours.
Also, if you’re reading this and you’re in a country where this is covered? Please, don’t take it for granted. Someone else is crying in a bathroom because they can’t afford it.
And yes, I’ve sent this link to three friends already. One of them just started methylnaltrexone last week. She sent me a voice note saying she cried again. This is powerful stuff.
Stay strong, everyone. You’re not alone. 💪❤️
kate jones
February 4, 2026 AT 11:32Peripherally acting mu-opioid receptor antagonists (PAMORAs) represent a pharmacologically elegant solution to a physiologically complex iatrogenic condition. The selective antagonism of peripheral mu-opioid receptors without central penetration is a triumph of receptor subtype specificity and pharmacokinetic engineering. The differential distribution profiles of methylnaltrexone (quaternary ammonium, poor BBB penetration), naloxegol (PEGylated naloxone derivative), and naldemedine (structural analog with enhanced polarity) reflect targeted molecular design principles that minimize off-target effects.
However, the clinical translation of these agents is hampered by socioeconomic determinants of access, not therapeutic efficacy. The persistent underutilization of PAMORAs in non-oncologic populations reflects systemic bias in pain management paradigms and insurance gatekeeping. The American Gastroenterological Association’s 35–40% access estimate is not a failure of medicine-it is a failure of policy.
Further research should investigate the gut-brain axis modulation by PAMORAs, particularly their potential influence on central pain processing via vagal afferents-a possible secondary benefit not yet quantified.
Natasha Plebani
February 5, 2026 AT 10:58It’s funny how we’ve turned constipation into a moral crisis. We’re told to ‘fight’ it, ‘overcome’ it, ‘take control’ of our bowels. But what if the real problem isn’t your gut-it’s the fact that we’ve built a system where pain relief requires you to sacrifice your dignity? Where the only way to feel human again is to spend $5,000 on a drug that doesn’t even work for everyone?
Maybe the real question isn’t ‘Which PAMORA?’
It’s ‘Why do we let pharmaceutical companies hold our comfort hostage?’
And why are we still surprised when the body rebels against being treated like a machine?
These drugs fix the symptom. But they don’t fix the system.
And maybe… that’s the real constipation.