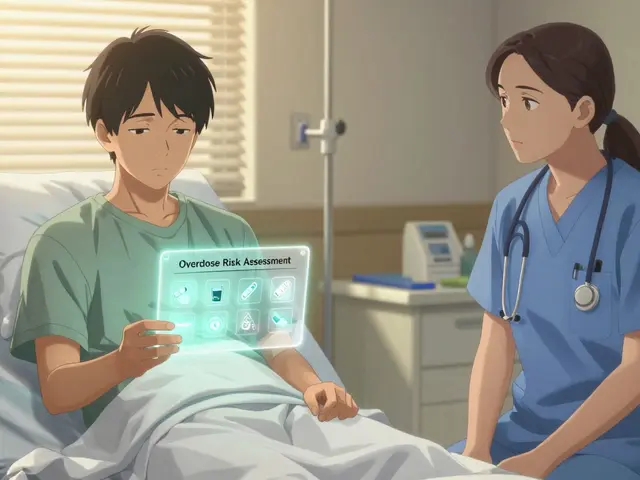
Getting the right dose of medicine for a child isn’t just tricky-it’s life-or-death. A wrong number, a mix-up between pounds and kilograms, or a missed dose can turn a simple illness into a medical emergency. Pediatric dosing apps and printed dosing charts aren’t just convenient tools-they’re essential safety nets in homes and hospitals alike. But not all apps are created equal. Some save lives. Others create new risks. Knowing which ones to use-and how to use them right-is critical.
Why Pediatric Dosing Is So Different
Adults usually take the same dose regardless of weight. Kids don’t. Their bodies process medicine differently. A 10-pound infant needs a fraction of what a 70-pound child takes. Even small mistakes can be dangerous. The Institute for Safe Medication Practices found that medication errors in children happen up to three times more often than in adults. Most of these errors come from manual calculations. A doctor, nurse, or parent trying to calculate a dose by hand under pressure is far more likely to get it wrong.That’s why weight-based dosing is the standard. But weight isn’t always easy to get right. Parents might guess. Clinicians might record it in pounds when the system expects kilograms. One wrong decimal point, one misread unit, and you’ve given a child 300% too much ibuprofen. That’s not theoretical-it happened in a real case documented in the Journal of Pediatric Pharmacology and Therapeutics in April 2024. The child survived, but barely.
Clinician Apps: Speed and Accuracy in Emergencies
In hospitals and ERs, time is everything. That’s where apps like Pedi STAT and Epocrates come in. Pedi STAT, developed in 2009 by emergency doctors at Connecticut Children’s, was built for one thing: stopping calculation errors during crises. Type in a child’s weight in kilograms, pick the drug-epinephrine, acetaminophen, antibiotics-and the app spits out the exact dose in seconds. No math. No guessing.Studies show it cuts calculation time from nearly 19 seconds to under 3. Error rates drop from over 12% to under 5%. In a code blue situation, those seconds matter. Pedi STAT has over 200 pediatric medications built in, including emergency dosing for seizures, anaphylaxis, and shock. It’s used in 89% of U.S. children’s hospitals today.
Epocrates is another go-to. It’s older, broader, and covers over 4,500 medications. It checks for dangerous drug interactions and cross-references with patient allergies. But it’s not built for emergencies. It’s better for routine inpatient or outpatient use. The free version gives basic dosing. The $175/year Plus version adds advanced alerts and formulary links.
These tools aren’t magic. They require training. A 2023 study found that 63% of users made errors when they entered weight in pounds instead of kilograms. That’s why hospitals now require staff to pass a quick competency test before using these apps on real patients. And every clinician is still taught to double-check the result manually-even if the app says it’s right.
Parent Apps: Keeping Kids Safe at Home
Most pediatric dosing errors happen at home-not in the hospital. Parents juggle multiple medications, irregular schedules, and sleep-deprived nights. A 2023 survey by the American Academy of Pediatrics found that 87% of dosing mistakes occurred during transitions: when a child came home from the ER, switched doctors, or started a new treatment.That’s where apps like My Child’s Meds and NP Peds MD step in. My Child’s Meds, endorsed by the Royal College of Paediatrics and Child Health, is designed for parents. It lets you log every medication, set reminders for doses, and track when each one was given. Color-coded icons show if a dose was given, missed, or doubled. It even flags if you’re about to give two medicines with the same active ingredient-like giving both Tylenol and a cold syrup that both contain acetaminophen.
One parent, Sarah K., wrote in her App Store review: “This app saved us from a potential overdose when my toddler’s fever reducer schedule got confusing during night feedings.” That’s the kind of real-world impact these tools have. User data from the app’s developers shows a 38% drop in parent-reported dosing errors and a 92% reduction in accidental double dosing.
NP Peds MD, developed by Northpoint Pediatrics, is simpler. It doesn’t send reminders. It doesn’t store records. But it gives you instant, verified dosage charts by weight for common OTC meds like ibuprofen and acetaminophen. You just select the child’s weight, and it shows you the exact amount to give. A 2024 Consumer Reports study found that 78% of parents using this app gave the right dose-compared to only 52% using printed paper charts.
The Big Problem: Apps Don’t Talk to Each Other
Here’s the catch: hospital apps and home apps don’t connect. A child leaves the ER with a paper handout. Mom opens My Child’s Meds and types in the dose manually. She misreads the handwriting. The hospital’s Pedi STAT system never synced with her phone. No one knows what’s been given at home. No one knows what’s been missed.This gap is dangerous. A 2023 WellChild survey found that 68% of parents struggled to transfer medication info from hospital to home. One parent in the survey entered her child’s weight as 44 pounds-when it was actually 20 kilograms (about 44 pounds). The app didn’t warn her. She gave the adult dose. The child was hospitalized.
Even worse, some apps are just glorified note-takers. Apps like Child Medical History cost $3.99 and let you log meds-but they don’t calculate anything. No safety checks. No alerts. Just a digital notebook. That’s not a tool. That’s a false sense of security.
What to Look for in a Pediatric Dosing App
Not all apps are safe. Here’s how to tell the good ones from the risky ones:- Check the source. Is it made by a hospital, pharmacy group, or pediatric association? My Child’s Meds was co-developed with the Royal College of Paediatrics and Child Health. That’s a red flag for legitimacy.
- Look for clinical validation. Does the app cite studies or guidelines? Does it reference the Harriet Lane Handbook or AAP dosing standards? If it doesn’t, walk away.
- Watch for unit warnings. Good apps automatically ask if your weight is in kg or lb-and convert it correctly. Bad apps assume one and don’t warn you.
- Avoid free apps with no name. If you downloaded it from an unknown developer and it doesn’t say who made it, it’s not trustworthy.
- Don’t rely on it alone. Always cross-check the dose with the prescription label or pharmacy instructions. Apps can glitch. Phones die. Paper backups are non-negotiable.
Best Practices for Parents and Clinicians
Whether you’re a nurse or a mom, these steps will keep your child safe:- Always confirm weight in kilograms. Most clinical apps use kg. If you’re entering weight, double-check the unit. Convert pounds to kg by dividing by 2.2.
- Use one app only. Don’t juggle three different apps. Pick the best one for your role-My Child’s Meds for home, Pedi STAT for hospital.
- Update regularly. App updates fix bugs and add new drug guidelines. Turn on auto-updates.
- Keep a paper list. Write down every medication, dose, time, and reason. Bring it to every appointment. Hospitals still rely on paper during power outages.
- Reconcile weekly. Compare your app’s log with your pharmacy’s refill record. If they don’t match, call your pediatrician.
- Teach everyone who gives meds. Grandparents, babysitters, nannies-they all need to know how the app works. Don’t assume they’ll figure it out.
The Future: Smarter, Safer Systems
The next wave of pediatric dosing tech is coming fast. Pedi STAT is testing AI that predicts when a parent is likely to make a mistake-based on time of day, past errors, and sleep patterns. Boston Children’s Hospital is trialing smart pill dispensers that only unlock the right dose at the right time. And HIMSS is building a new data standard to let hospital apps talk to parent apps-finally closing the gap between clinic and home.By 2027, 95% of pediatric doses in hospitals will be verified digitally. That’s huge. But tech alone won’t fix this. Education will. Training will. Double-checking will.
Apps are tools-not replacements for thinking. The best dose tracker is still the one in your head: know your child’s weight, know the drug, know the dose. Use the app to confirm, not to decide.
Can I use any medication app for my child?
No. Only use apps developed by trusted medical institutions like hospitals, pediatric associations, or pharmacy groups. Avoid generic health apps or those without clinical validation. Apps like My Child’s Meds and NP Peds MD are backed by pediatric experts. Free apps with no clear developer are risky and may give incorrect doses.
Do I still need paper dosing charts if I use an app?
Yes. Always keep a printed copy of your child’s medication schedule. Phones die, apps crash, and power outages happen. Paper is your backup. Write down each drug, dose, time, and reason. Bring it to every doctor visit and emergency room trip.
What’s the difference between Pedi STAT and My Child’s Meds?
Pedi STAT is for healthcare professionals in emergencies. It calculates doses for 200+ medications in seconds and is used in hospitals. My Child’s Meds is for parents at home. It tracks doses, sends reminders, and prevents double dosing. They don’t connect. Use each for its intended purpose.
Why do some apps ask for weight in kilograms and others in pounds?
Clinical apps like Pedi STAT use kilograms because that’s the global medical standard. Parent apps may let you choose, but you must be careful. Entering weight in pounds when the app expects kg can cause a 2.2x overdose. Always check the unit before entering data. If in doubt, convert: divide pounds by 2.2 to get kilograms.
Are pediatric dosing apps safe from hackers?
Clinical apps like Pedi STAT and Epocrates are HIPAA-compliant and encrypted. Parent apps like My Child’s Meds are designed for personal use and don’t store data in the cloud-so your child’s info stays on your phone. Avoid apps that ask for unnecessary permissions or require accounts. If it doesn’t mention privacy or security, assume it’s not safe.
What should I do if my child gets the wrong dose?
Call Poison Control immediately at 1-800-222-1222 (U.S.) or your local emergency number. Don’t wait for symptoms. Have the medication name, dose given, child’s weight, and time of ingestion ready. If you used an app, show the screen to medical staff. It helps them assess the risk faster.
Next Steps: What to Do Today
If you’re a parent: Download My Child’s Meds or NP Peds MD. Enter your child’s current medications. Set reminders. Print a copy. Share it with caregivers.If you’re a clinician: Make sure your hospital uses Pedi STAT or Epocrates. Get trained. Never skip the manual check. Advocate for better integration with home apps.
If you’re a caregiver: Always confirm the weight unit. Always double-check the dose. Always have a paper backup. Safety isn’t about technology-it’s about habits. Build them now, before the next fever hits.





Prem Hungry
November 17, 2025 AT 13:12man i just downloaded np peds md after readin this… been usin paper charts for my lil one n almost gave her double dose last week bc i was half asleep. this app is a lifesaver. no more guesswork. ty for the post!!
Leslie Douglas-Churchwell
November 18, 2025 AT 21:57Let me just say-this entire post is a masterclass in medical paternalism wrapped in a techno-solutionist bow. 🤦♀️ We’re being sold ‘apps’ like they’re sacraments while Big Pharma quietly lobbies to keep interoperability standards *deliberately* fragmented. Did you know Pedi STAT’s parent company has ties to Medtronic? And My Child’s Meds? Their ‘clinical validation’ is just a letter from a consultant who used to work at Johns Hopkins. 🧪 The real issue? No one’s auditing algorithmic bias in weight conversions for non-Western body types. This isn’t safety-it’s surveillance capitalism with a pediatric veneer. 🚨
shubham seth
November 20, 2025 AT 11:20bro this post is pure gold. i’m a nurse in delhi and we use epocrates like it’s gospel-until some intern types in 44 lbs and the app says 120mg of amoxicillin. 44 lbs = 20kg, but the app didn’t flag it. kid got 3x the dose. we saved him, but holy hell. apps are tools, not oracles. if you don’t know how to convert kg/lb, you shouldn’t be touching the phone. period. also-why the hell are we still using pounds in the US? it’s 2024. metric is not a suggestion.
Kathryn Ware
November 21, 2025 AT 02:40Thank you for this incredibly thorough breakdown-I’ve been advocating for better pediatric dosing tools in my hospital for years, and this nails every pain point. 💡 I especially appreciate the emphasis on cross-checking with paper backups. Last month, our EHR went down during a code, and the nurse who had printed the child’s med list (including weight in kg and all doses) was the only one who didn’t panic. Also-yes, please teach EVERYONE who touches the meds! My sister-in-law thought ‘acetaminophen’ was just ‘Tylenol’ and gave both at the same time. My child’s app flagged it immediately, but not all parents have that luxury. The AI predictive feature Pedi STAT is testing? That’s the future. Imagine an app that notices you’ve been up for 36 hours and says, ‘Hey, you’re exhausted. Don’t trust your math right now. Call Poison Control.’ That’s empathy engineering. 🙏
Jessica Healey
November 21, 2025 AT 19:56i hate how everyone acts like apps are magic… my cousin’s kid died from a wrong dose and it was because they trusted some random app from the app store. i cried for weeks. now i only use paper. no tech. no phones. just me, a pen, and my baby’s weight written on a sticky note. no one can hack a sticky note.
Levi Hobbs
November 22, 2025 AT 02:35Yes, yes, YES to the paper backup. I’ve been telling my coworkers for years: the app might crash, the battery might die, the Wi-Fi might be down-but a laminated card taped to the fridge? That’s forever. Also-don’t forget to update the list after every pharmacy refill. I once had a parent come in with a 3-month-old list that included a discontinued antibiotic. We almost gave it again. 😳
henry mariono
November 23, 2025 AT 03:32Appreciate the post. I’ve been using My Child’s Meds for 8 months now. It’s quiet, reliable, and doesn’t nag. I keep the paper list in my purse. I don’t need to shout about it. Just doing the work. That’s enough.
Sridhar Suvarna
November 24, 2025 AT 16:20India needs this badly. So many parents here use Google Translate to read labels. One mom gave her 2-year-old adult ibuprofen because the app said '200 mg' and she thought it was for kids. No unit warning. No voice alert. Just text. We need low-literacy apps-simple icons, voice input, local language support. This isn't just tech-it's public health. Let's build for the 80%, not the 20% with iPhones.
Joseph Peel
November 26, 2025 AT 04:52As someone who grew up in a household where medicine was measured with kitchen spoons, I can’t express how grateful I am for these tools. But the real hero here isn’t the app-it’s the parent who reads the label twice, who calls the pharmacy, who writes it down. Technology helps. But vigilance? That’s the real medicine.