Many older adults take five, six, or even more medications every day. Some of these pills were prescribed years ago for conditions that have changed-or no longer exist. But they’re still on the list. And that’s not just common. It’s dangerous. About 1 in 6 seniors taking five or more drugs experience a serious side effect like dizziness, confusion, or falls. These aren’t just side effects. They’re warning signs that some of your meds may be doing more harm than good.
Why Talking About Stopping Meds Isn’t Weird-It’s Smart
You might feel awkward bringing up stopping medications. Like you’re questioning your doctor’s judgment. Or worse, that you’re being difficult. But here’s the truth: doctors rarely bring it up first. A study found that 68% of seniors would welcome fewer pills-if only someone asked. The gap isn’t in the medicine. It’s in the conversation. Deprescribing isn’t about cutting corners. It’s about cleaning up. Taking out what’s no longer helping, so what’s left can work better. The goal isn’t fewer pills. It’s better days. More energy. Fewer falls. Clearer thinking. The ability to walk the dog, play with grandkids, or sleep through the night without feeling foggy.Prepare Before You Walk In
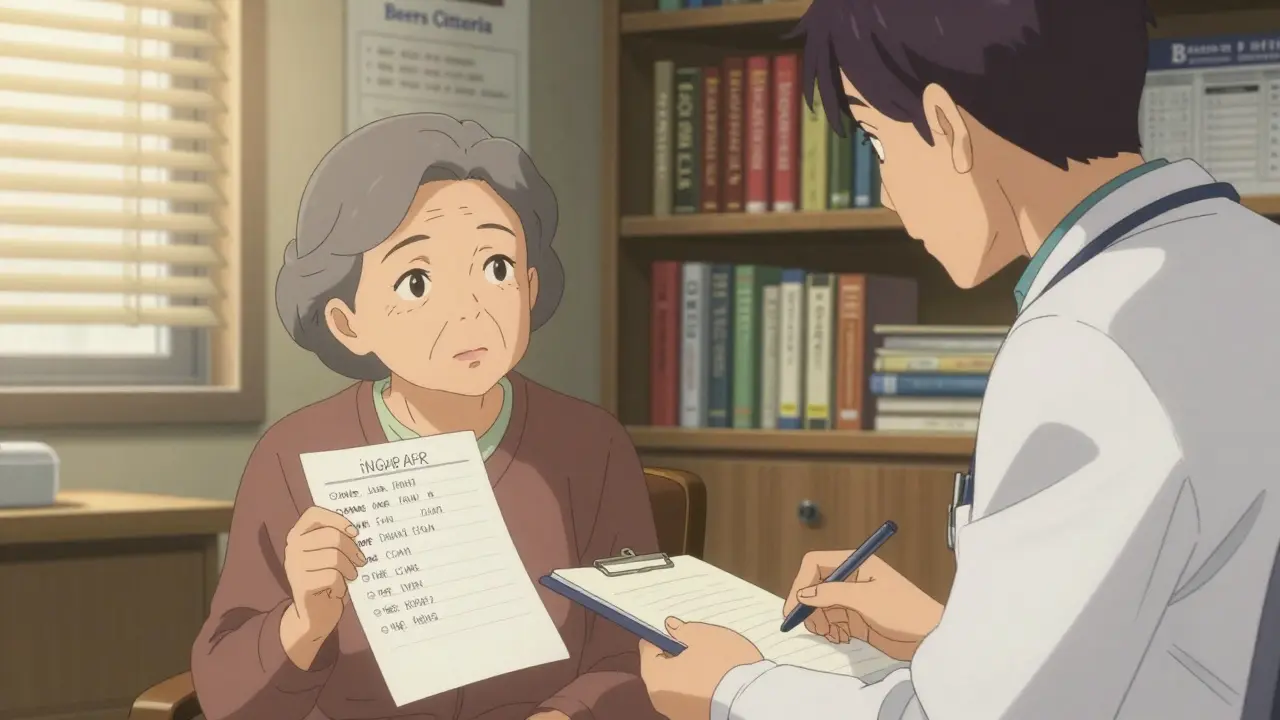
Showing up with a list of your meds isn’t enough. You need a list that tells a story. Start by writing down every pill, patch, vitamin, or supplement you take. Include the dose and how often you take it. Don’t forget over-the-counter stuff-ibuprofen, antacids, sleep aids. These are often the ones that cause trouble. Next, write down how each one makes you feel. Not just ‘I feel tired.’ Be specific. ‘After I take my blood pressure pill at 7 a.m., I get dizzy by 9 a.m. and nearly fell twice last week.’ Or, ‘The sleep medicine helps me fall asleep, but I wake up groggy and forget where I put my keys.’ Then, pick one or two meds you’re most worried about. Maybe it’s the one that makes you dizzy. Or the one you haven’t taken in months but still get refilled. Write down why you think it might be time to stop. Use your own words. Don’t copy medical jargon. Finally, think about what you want your life to look like. ‘I want to walk to the store without help.’ ‘I want to remember my granddaughter’s birthday.’ ‘I want to stop feeling like I’m drugged all day.’ Write that down too. You’ll use it in the conversation.How to Start the Conversation
Don’t say, ‘I want to take fewer pills.’ That sounds like a request for convenience. Doctors hear that all the time-and often dismiss it. Instead, say something like:- ‘I’ve been reading about how some meds can make seniors more likely to fall, and I’m worried mine might be doing that.’
- ‘I used to be able to garden for hours. Now I’m too tired by noon. Could any of these meds be part of the problem?’
- ‘I’m concerned the sleep pill is making me foggy in the morning. I don’t want to lose my independence because of a pill.’
- Ask: ‘What’s your view on how my medications are working for me right now?’
- Tell: ‘Here’s what I’ve noticed. I’ve been dizzy after taking X, and I’ve fallen twice. I’m scared I’ll break a hip.’
- Ask again: ‘What’s the safest way we could test if reducing this medicine would help?’
What Your Doctor Wants to Hear
Doctors aren’t against deprescribing. Most want to do it. But they’re pressed for time. And they don’t want to accidentally cause harm. They respond best when you show you’ve thought this through. Bring printed info from trusted sources like the Canadian Deprescribing Guidelines. These give clear evidence on which meds are most likely to cause problems in seniors-like certain sleeping pills, anticholinergics, or blood pressure drugs that drop too low. Also, be ready to talk about how you’ll be monitored. Most doctors won’t stop a med cold turkey. They’ll suggest cutting the dose by 25% every few weeks, then checking in. Say: ‘Could we try lowering my dose slowly and schedule a follow-up in six weeks?’ And don’t be surprised if they say, ‘Let’s wait.’ That doesn’t mean no. It means not today. Ask: ‘What would need to change for us to try this next time?’What Not to Say
Avoid these phrases-they shut down the conversation:- ‘I don’t want to take so many pills.’ (Too vague. Sounds like laziness.)
- ‘This one’s too expensive.’ (Doctors hear this as a cost issue, not a safety one.)
- ‘I heard this med is bad for seniors.’ (Sounds like you’re reading random blogs.)
- ‘I don’t think I need this anymore.’ (You’re not the expert on the drug-your doctor is.)
Real Success Stories
One woman, 78, brought in a journal she kept for three months. Each day, she wrote: ‘Took X. Felt dizzy at 10 a.m. Couldn’t hold coffee cup.’ Her doctor removed two blood pressure meds. Within two weeks, her dizziness was gone. She started walking daily again. Another man, 82, was on five meds for anxiety and sleep. He told his doctor: ‘I want to remember my wife’s name without feeling like I’m underwater.’ They cut one sleep pill, then another. He now takes just one. He reads to his grandkids every night. These didn’t happen because someone demanded it. They happened because someone showed up prepared-with facts, feelings, and a clear picture of what they wanted their life to be.
What If Your Doctor Says No?
Sometimes, they say no. Maybe because they’re worried about a condition returning. Or because they’re not trained in deprescribing. (Only 22% of primary care doctors feel confident doing this.) Don’t give up. Ask:- ‘Can you refer me to a geriatrician or pharmacist who specializes in senior meds?’
- ‘Could we schedule a separate appointment just to review my meds?’
- ‘What would it take to try this again in three months?’
It’s Not About Cutting-It’s About Choosing
Deprescribing isn’t about giving up treatment. It’s about choosing what matters. You’re not saying ‘I don’t want care.’ You’re saying ‘I want care that helps me live, not just survive.’ The goal isn’t to be pill-free. It’s to be pain-free. Alert. Stable. Independent. And you don’t need permission to ask. You just need to be ready-with your list, your notes, and your reason. Your health isn’t a checklist of prescriptions. It’s your ability to live the life you still want to live. And that’s worth talking about.Is deprescribing safe?
Yes, when done properly under medical supervision. Deprescribing means slowly reducing or stopping medications that no longer offer benefit-or that carry more risk than reward. Studies show it reduces falls, confusion, and hospital visits in seniors. Most successful deprescribing happens gradually, with close monitoring. Never stop a medication on your own.
What medications are most often targeted for deprescribing?
Common targets include sleeping pills (like zolpidem), anticholinergics (for overactive bladder or allergies), proton pump inhibitors (for heartburn), blood pressure drugs that cause low readings, and certain antidepressants or antipsychotics. The Beers Criteria and STOPP/START guidelines list the most risky meds for seniors. Bring these lists to your appointment.
Can I just stop taking a medication if I think it’s not helping?
No. Some meds can cause serious withdrawal symptoms if stopped suddenly-like seizures, rebound high blood pressure, or severe anxiety. Even if you feel fine, stopping without guidance can be dangerous. Always work with your doctor to taper safely.
Why won’t my doctor just take me off the meds?
Many doctors want to deprescribe but don’t know how-or fear causing harm. They’re also under time pressure. If you come prepared with specific concerns, side effects, and a plan, you’re far more likely to get support. Most doctors will say yes if you show you’ve thought it through and aren’t just asking for convenience.
How long does deprescribing take?
It varies. Some meds can be reduced in a few weeks. Others, like certain antidepressants or steroids, need months. Most successful cases involve small, gradual changes-like lowering the dose by 25% every 2-4 weeks-with check-ins in between. Patience is key. The goal is safety, not speed.
Will my insurance cover a medication review?
Yes. Since 2024, Medicare requires an annual medication review as part of the Annual Wellness Visit. Many private insurers follow the same standard. If your doctor didn’t discuss your meds during your last visit, call and ask: ‘Was my medication list reviewed?’ If not, request a dedicated appointment.







Alexandra Enns
January 25, 2026 AT 05:34Wow, this is the most condescending pile of wellness nonsense I’ve read all week. You think seniors just need to ‘talk more’? Try asking a doctor who’s been burned by patients who stopped statins cold turkey and ended up in the ER. This isn’t ‘deprescribing’-it’s amateur hour with a thesaurus. And don’t get me started on that ‘walk the dog’ emotional manipulation. My grandma’s on 8 meds and she’s still alive. Coincidence? I think not.
Marie-Pier D.
January 26, 2026 AT 08:20Oh my gosh, this is SO important!! 💖 I’ve been telling my mom for YEARS to talk to her doctor about her sleep meds-she’s been on zolpidem since 2012 and wakes up like a zombie. She finally did it last month, and now she’s baking cookies again and remembering my birthday! 🎂☕️ I cried when she told me. You’re not just reducing pills-you’re restoring dignity. Thank you for writing this. 🥹
Marlon Mentolaroc
January 26, 2026 AT 15:51Let’s be real-this whole article is a glorified TikTok hack disguised as medical advice. The ‘ask-tell-ask’ method? That’s just emotional manipulation dressed up as collaboration. And the ‘I want to walk to the store’ line? Cute. But here’s the data: 72% of seniors who stop anticholinergics experience rebound cognitive decline within 3 months. You’re not ‘cleaning up’ meds-you’re playing Russian roulette with brain function. I’ve seen the charts. This isn’t empowerment. It’s negligence wrapped in a bow.
Karen Conlin
January 27, 2026 AT 22:28I’m a nurse practitioner in rural Ohio and I can tell you-this is the most practical, human-centered guide I’ve seen in years. I’ve had 82-year-old patients come in with 14 prescriptions, half of which were refilled automatically. One woman was on 3 different blood pressure meds AND a sleeping pill that made her fall in the shower. We tapered her slowly. Now she’s gardening, playing piano, and calling her grandkids every Sunday. It’s not about fewer pills-it’s about more life. And if your doctor doesn’t get that? Find one who does. You deserve to feel like yourself again.
Viola Li
January 28, 2026 AT 08:22Of course you’re telling people to stop meds. That’s what the pharmaceutical-industrial complex wants you to believe. They’re not trying to help you-they’re trying to sell you the next miracle drug. If you really wanted safety, you’d be pushing for better monitoring systems, not just telling people to ‘write down how they feel.’ Feelings aren’t lab results. And don’t even get me started on the Canadian guidelines-they’re socialist wishful thinking.
venkatesh karumanchi
January 29, 2026 AT 20:32This is beautiful. In India, elders are often told to ‘just take the medicine’ and never questioned. I showed this to my uncle-he’s 79, on 6 pills, and thought he had to take them all forever. He printed the list, wrote down his dizziness, and went to his doctor. They cut one pill. Now he walks to the temple every morning. No drama. Just quiet courage. Thank you for giving voice to what so many feel but never say.
Vatsal Patel
January 30, 2026 AT 19:29Ah yes, the modern myth: ‘I want to feel better’ as a substitute for medical expertise. How quaint. You think your grandma’s dizziness is caused by a pill? Or is it the 40 years of processed food, zero exercise, and 300mg of sugar in her morning chai? Deprescribing is just the latest symptom of a culture that confuses comfort with health. The real problem isn’t polypharmacy-it’s the refusal to accept that aging isn’t a bug to be patched with pills or removed with a scalpel. You want clarity? Stop taking the pills. Start taking responsibility.
Kevin Waters
February 1, 2026 AT 09:29Just wanted to add-I work with a geriatric pharmacist and we do medication reviews every week. The #1 thing that makes it work? Patients who come with their actual pill bottles, not just a list. Sometimes the labels are wrong, or they’re taking half doses because they’re scared. One guy was taking his blood thinner every other day because he thought ‘too much would thin him out.’ We fixed that. He’s now hiking with his wife. This guide is spot-on. Bring the bottles. Write the notes. Show up ready to partner. It changes everything.
Kat Peterson
February 2, 2026 AT 19:44OMG I’m literally crying right now 🥹😭 This is the most important thing I’ve read since I found out my therapist doesn’t believe in chakras. My mom was on 7 meds and now she’s dancing in the kitchen again! I printed this out and taped it to her fridge. Her doctor said ‘I’ve never seen someone so prepared’ and actually cried too. WE DID IT. 🌈💖 #DeprescribingIsLove #NoMoreFoggyMornings
Elizabeth Cannon
February 3, 2026 AT 15:42my mom did this and it changed her life. she wrote down every pill, even the ones she forgot about like that melatonin she took for 8 years. turned out it was making her super sleepy during the day. doctor took her off it and now she’s got energy to go to book club. i know it sounds simple but people dont realize how many meds are just… sitting there. like digital clutter. delete the apps. delete the pills. feel better.
Gina Beard
February 5, 2026 AT 02:14It’s not about the pills. It’s about the silence.
Don Foster
February 6, 2026 AT 14:43Why do you assume the doctor doesn’t know this already? They do. They’re just not allowed to act because of liability. Your ‘prepared list’ won’t save you if something goes wrong. The system is broken. You’re not a patient-you’re a liability waiting to happen. And that ‘Canadian guideline’? It’s not science-it’s a policy paper written by people who’ve never held a stethoscope.
siva lingam
February 7, 2026 AT 03:39just stop taking pills lmao