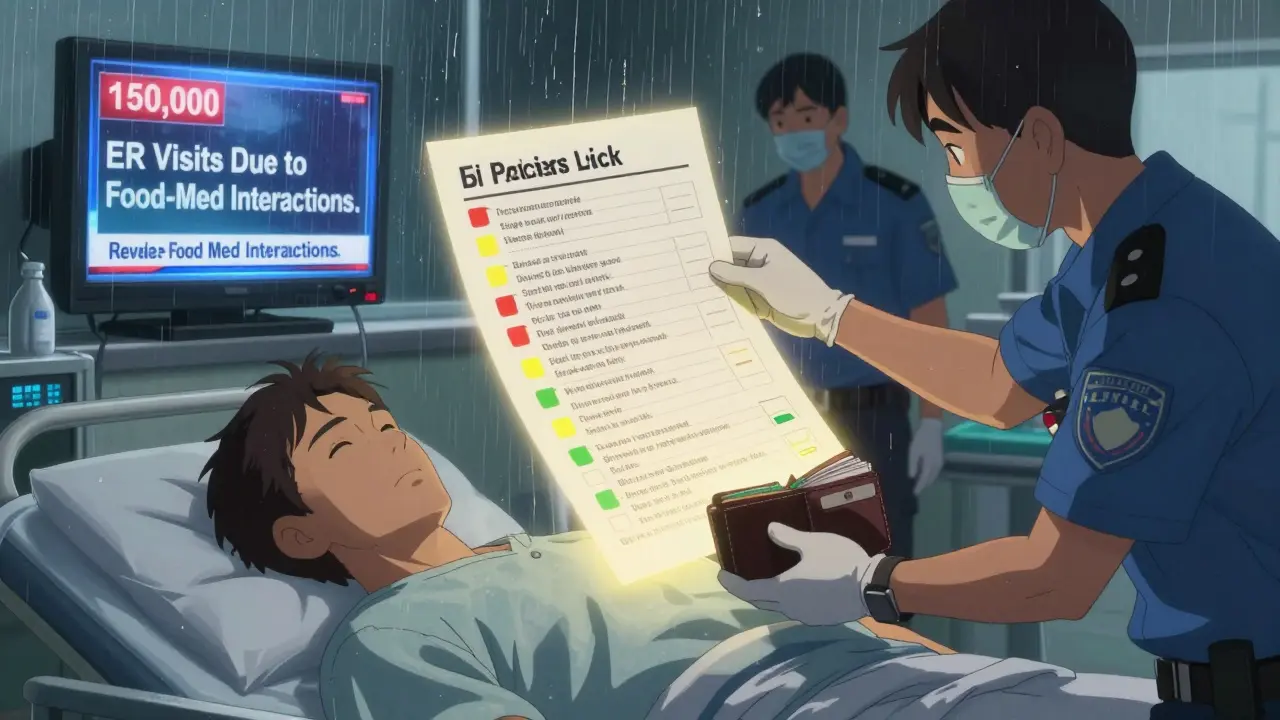
Every year, over 150,000 people in the U.S. end up in the emergency room because of food and medication interactions. Many of these cases are preventable. If you’re taking even one prescription drug, supplement, or over-the-counter medicine, you’re at risk. A simple checklist kept at home can stop dangerous reactions before they happen. This isn’t just for seniors or people on dozens of pills. It’s for anyone who eats and takes medicine - and that’s almost everyone.
Why Your Medicine Might Not Work (or Could Hurt You)
Medications don’t just float around your body in a vacuum. They react with what you eat and drink. Grapefruit juice can make cholesterol drugs like simvastatin 300-500% stronger, leading to muscle damage or kidney failure. Dairy products like milk and yogurt can block antibiotics like ciprofloxacin from being absorbed, making them useless. Even something as simple as a spinach salad can interfere with blood thinners like warfarin - not because it’s bad, but because too much or too little vitamin K throws your dose off balance.
The FDA reports that 12% of all adverse drug events involve food or drink. That’s not rare. It’s common. And most people don’t know it’s happening. You might think, “I’ve been taking this pill with breakfast for years.” But if your diet changed - maybe you started juicing kale, switched to plant-based milk, or began taking fish oil - your risk just went up.
What Goes on the Checklist
A good checklist isn’t just a list of pills. It’s a living document that answers three questions: What are you taking? What should you avoid? And what happens if you mess up?
For each medication, include:
- Drug name - both brand (Coumadin) and generic (warfarin)
- Dosage and schedule - “5 mg once daily at 8 a.m.”
- Purpose - “Prevents blood clots after knee surgery”
- Prescribing doctor - Name and clinic number
- Food or drink interaction - “Avoid grapefruit juice,” “Take 2 hours before or after dairy,” “Keep vitamin K intake consistent”
- Risk level - High, Moderate, or Low
- Source - “FDA Drug Safety Communication #2024-087” or “NZ Formulary, July 15, 2024”
Don’t forget supplements. People think “natural” means safe, but garlic, ginkgo, and St. John’s wort all interact with common drugs. Even vitamin E can thin your blood when combined with warfarin. List them like medications.
How to Rate the Risk
Not all interactions are equal. You need to know which ones can kill you and which ones just need a little timing adjustment.
- High Risk - Can cause immediate danger. Examples: Grapefruit juice with statins, tyramine-rich foods (aged cheese, cured meats) with MAO inhibitors like tranylcypromine. Strict avoidance required.
- Moderate Risk - Reduces effectiveness or causes side effects if timing is wrong. Examples: Dairy with antibiotics, calcium supplements with thyroid meds. Separate by 2-4 hours.
- Low Risk - Minor or only risky with large amounts. Examples: Leafy greens with warfarin - keep intake steady, don’t quit them cold. Monitor, don’t avoid.
Use color coding: red for high, yellow for moderate, green for low. If you’re printing this, use highlighters. If you’re using an app, tag each interaction. This makes it easy to scan in a hurry.
Where to Get Accurate Info
Google isn’t enough. Many websites give outdated or wrong advice. Stick to these trusted sources:
- FDA Drug Safety Communications - Look up your drug by name on fda.gov
- New Zealand Formulary Interaction Checker - Free, updated monthly, used by pharmacists worldwide
- SEFH Drug-Food/Herb Interaction Guide (2024 edition) - Laminated cards you can stick on your fridge
- Your pharmacist - Ask them to review your list during your next refill. Most will do it for free.
Never trust a blog post, Reddit thread, or YouTube video. Even if it sounds right, it might be missing key details. For example, one Reddit user thought kale was dangerous with warfarin - but didn’t realize that cooked spinach has 70% less vitamin K than raw. That’s the kind of detail that saves lives.
Paper vs. Digital: Which Should You Use?
There’s no one-size-fits-all. Here’s what works for different people:
| Feature | Paper Checklist | Digital App |
|---|---|---|
| Accessibility | Works anywhere - no battery, no signal | Needs phone, app, and internet |
| Updates | You must rewrite it manually | Auto-updates from drug databases |
| Emergency use | EMS and ER staff can read it instantly | Hard to access if phone is locked or dead |
| Adoption rate (65+) | 92% | 63% |
| Error reduction | 37% | 42% |
If you’re over 70 or live in a rural area, go paper. If you take five or more meds and change them often, use an app like Medisafe or MyTherapy. Best option? Keep both. Use the paper version as your emergency backup. Keep the digital one for daily tracking.
How to Build It - Step by Step
Start with 30-45 minutes. You don’t need to do it all at once, but finish it within a week.
- Gather everything. Pull out all pills, bottles, supplements, and OTC meds. Don’t skip the aspirin or melatonin.
- Write down each one. Use the 6-item format above. Include exact doses and times.
- Look up each interaction. Use the FDA or NZ Formulary. Don’t guess. If you’re unsure, call your pharmacist.
- Assign risk levels. Red, yellow, green. Be honest - if it’s dangerous, mark it high.
- Write your emergency contacts. Two people who know your meds. Include their phone numbers.
- Write your allergies. Not just “penicillin.” Say “anaphylaxis, swelling, trouble breathing.”
- Put it where you’ll see it. Fridge door. Bathroom mirror. Wallet. Don’t hide it in a drawer.
- Update it every month. Link it to your refill day. If your doctor changed your dose, update the list.
What to Do When You’re Sick or See a New Doctor
Don’t wait for them to ask. Hand them your checklist before they even sit down. Most doctors won’t ask about food interactions unless you bring it up. A 2024 study found that patients who brought their own medication lists had 78% better communication with providers.
If you’re going to the ER, tape a copy to the inside of your wallet. Or put it in your phone’s emergency contact info. First responders are trained to look there.
Common Mistakes (And How to Avoid Them)
- “I don’t need to update it - I’m on the same meds.” You’re not. Your doctor added a new pill. You started a new supplement. Update it.
- “I’ll remember.” You won’t. Memory fails under stress, illness, or sleep deprivation.
- “It’s just one grapefruit.” One grapefruit can affect your meds for 72 hours. It’s not about quantity - it’s about chemistry.
- “My app says it’s fine.” Apps miss regional foods. If you eat kimchi, natto, or fermented soy, your app might not know.
- “I don’t take supplements.” Do you take vitamin D? Fish oil? Ginger tea? Those count too.
Real Stories - What Happens When You Do This Right
A man in Ohio was on tacrolimus after a liver transplant. He drank grapefruit juice every morning. His doctor didn’t warn him. He ended up in the hospital with kidney failure. After he got out, he made a checklist. He now keeps it taped to his coffee maker. He hasn’t had a problem since.
A woman in Texas took warfarin. She loved kale smoothies. One week she had three. The next, none. Her INR spiked. She went to her pharmacist, who showed her how to keep vitamin K steady - one cup of cooked greens daily. She added it to her checklist. Her blood levels stabilized.
These aren’t rare cases. They’re everyday stories. And they all started with a checklist.
What’s Next
The FDA is rolling out new tools in 2025 - interactive checklists built into electronic health records. Smart fridges will soon scan your groceries and warn you if you’re about to buy something that clashes with your meds. But none of that matters if you don’t have your own baseline.
Right now, the best tool you have is your own hands. A pen. A piece of paper. Or a phone app. Start today. Don’t wait for a hospital visit. Don’t wait for a bad reaction. Build your checklist now - before you need it.
Do I need a checklist if I only take one medication?
Yes. Even one medication can interact with food. Grapefruit juice affects over 85 drugs. Warfarin interacts with dozens of foods. You don’t need to be on a dozen pills to be at risk. One interaction is enough to cause serious harm.
Can I just ask my doctor during my appointment?
You can, but most doctors have only 10-15 minutes per visit. They won’t have time to review every food interaction. Pharmacist-led medication reviews are better for this. Many Medicare Advantage plans cover them for free. Ask your pharmacist to go over your list - they’re trained for this.
What if I eat a food that’s on my high-risk list by accident?
Don’t panic. If it’s a one-time slip-up, monitor yourself. For high-risk items like tyramine with MAO inhibitors, watch for sudden headache, chest pain, or high blood pressure. If you feel anything unusual, call your doctor or go to urgent care. Keep a log of what you ate and when. That info helps them decide if you need action.
Are there foods that are safe for everyone?
Yes - but only if you’re not on interacting meds. Water, plain rice, apples, and plain bread are generally safe. But if you’re on lithium, salt-heavy foods can raise your levels. If you’re on diuretics, potassium-rich foods like bananas can become dangerous. There’s no universal “safe” list. Your checklist is your only reliable guide.
How often should I update my checklist?
Update it every time your meds change - new prescription, stopped pill, new supplement. Even if nothing changed, review it monthly. Link it to your refill day. Outdated lists cause 28% of errors, according to the FDA. Keeping it current is the single most important thing you can do.
Can I use a free template from the internet?
Yes - but only from trusted sources. Use the FDA’s “My Medicines” template (fda.gov/MyMedicines) or the American Heart Association’s 2024 printable version. Avoid random PDFs from blogs. They often miss key interactions or use outdated data. Stick to official health agency templates.







Kathy McDaniel
January 27, 2026 AT 20:12Paul Taylor
January 29, 2026 AT 02:21April Williams
January 30, 2026 AT 14:26suhail ahmed
January 31, 2026 AT 04:58Candice Hartley
February 2, 2026 AT 01:19astrid cook
February 3, 2026 AT 06:00Andrew Clausen
February 4, 2026 AT 08:51Anjula Jyala
February 6, 2026 AT 04:24Kirstin Santiago
February 6, 2026 AT 19:15Conor Murphy
February 7, 2026 AT 08:02Desaundrea Morton-Pusey
February 8, 2026 AT 19:20Murphy Game
February 8, 2026 AT 23:03Kegan Powell
February 9, 2026 AT 08:49