GLP-1 Nausea Tracker & Management Tool
Daily Nausea Tracker
Log your symptoms to identify patterns and get personalized recommendations
Your Progress
Personalized Recommendations
Pro Tip: Try ginger chews or acupressure wristbands for quick relief. Studies show they reduce nausea by up to 62%.
When you start a GLP-1 medication like Ozempic, Wegovy, or Mounjaro, the goal is clear: better blood sugar control, meaningful weight loss, and improved long-term health. But for many, the first few weeks bring something unexpected - persistent, sometimes debilitating nausea. It’s not rare. In fact, GLP-1 nausea affects up to half of users in the early stages, and for 1 in 10, it’s enough to quit the medication entirely. The good news? Most of it can be managed - and often avoided - with simple, science-backed strategies.
Why GLP-1 Medications Cause Nausea
GLP-1 receptor agonists work by mimicking a natural hormone that tells your body to slow down digestion. That’s helpful for controlling blood sugar and making you feel full longer. But it also means food sits in your stomach longer than usual. This delay in gastric emptying - sometimes slowed by 30% to 50% - is the main reason you feel nauseous. It’s not your imagination. It’s physiology. The nausea usually hits hardest in the first 4 to 5 weeks after starting the drug or after a dose increase. For most people, it fades within 8 days of starting. But if you jump too fast to higher doses, or eat the wrong foods, it can stick around much longer. Some patients report nausea lasting 10 weeks or more - not because the drug is broken, but because their body didn’t get time to adjust.Small Meals Are the First Line of Defense
If you’re eating three large meals a day, you’re asking your slowed-down stomach to handle more than it can. That’s like trying to fit a truckload of groceries into a compact car. The result? Discomfort, bloating, and nausea. The fix? Eat smaller portions, more often. Experts recommend cutting meal sizes by 25% to 30% and spreading your calories across 5 to 6 mini-meals instead of 3 big ones. Each meal should be around 300 to 400 calories. That’s about a small chicken breast, half a cup of rice, and a side of steamed veggies - not a full plate. Avoid high-fat foods. Fatty meals take even longer to digest, and when your stomach is already moving slowly, they’re a recipe for trouble. Skip fried chicken, heavy cream sauces, butter-heavy pastries, and full-fat cheese. Stick to lean proteins, whole grains, and vegetables. Bland carbs like plain toast, crackers, or oatmeal are especially helpful for morning nausea.Timing Your Drinks Makes a Big Difference
Drinking fluids with meals might feel natural, but it’s one of the biggest mistakes people make. Liquid adds volume to your stomach, which stretches it further - and when your stomach is already slow, that stretch triggers nausea. Instead, drink water or tea 30 to 60 minutes before or after eating. Sip slowly. Avoid gulping. Many patients report immediate relief after making this switch. One 45-year-old woman in a case study went from 5 to 6 nausea episodes a day to just 1 or 2 a week simply by separating her fluids from her meals.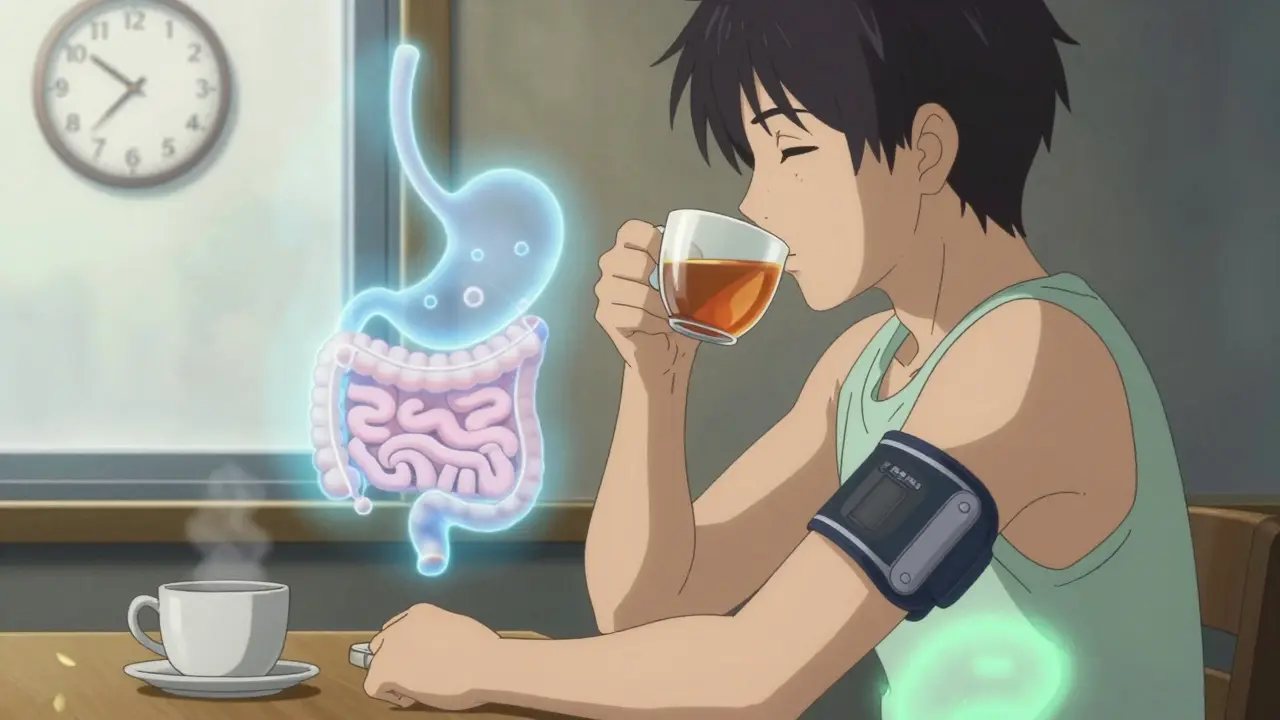
Try Ginger, Peppermint, and Acupressure
Some of the most effective tools for GLP-1 nausea aren’t drugs - they’re simple, natural remedies. Ginger has been shown in multiple studies to reduce nausea by up to 62%. Keep ginger chews, ginger tea, or ginger capsules on hand. Suck on a ginger lozenge at the first sign of queasiness. Peppermint works too - about 55% of users in small trials found relief with peppermint tea or oil. Both are safe, inexpensive, and don’t interfere with your medication. Acupressure wristbands, like Sea-Bands, are another underrated tool. A 2023 pilot study tracked 31 people on GLP-1 drugs and found these bands provided relief within 5 to 20 minutes in 80% of nausea episodes. They’re drug-free, reusable, and worn like a bracelet. No side effects. No prescriptions. Just pressure on a point on your wrist that’s been used for centuries to ease nausea.Slow Titration Is the Secret Weapon
The biggest mistake most people make? Rushing the dose increases. The manufacturer’s guidelines say to increase your dose every 2 to 4 weeks. But real-world data shows that’s too fast. Clinics that extend the time between dose increases to 6 weeks see nausea-related discontinuation rates drop from 12% to under 4%. Stay on your starter dose - 0.25 mg for semaglutide, 2.5 mg for tirzepatide - for at least 6 weeks. Don’t move up just because the calendar says so. Wait until your body feels settled. If nausea lingers, stay put. Your body isn’t failing. It’s adapting. One patient on Drugs.com increased Wegovy from 1.7 mg to 2.4 mg in just 4 weeks. The nausea lasted 11 weeks. Another patient stayed on 0.5 mg for 8 weeks before moving up. Their nausea lasted 3 days.When You Need Medication for Nausea
If diet and timing aren’t enough, and nausea is keeping you from eating, sleeping, or functioning - talk to your doctor about antiemetics. Domperidone is the top choice for most doctors. It helps your stomach empty faster without the neurological side effects of older drugs like metoclopramide. A typical dose is 10 to 20 mg, taken 3 to 4 times a day, 30 minutes before meals. It’s not perfect - the FDA has flagged rare heart risks with long-term use - but for short-term relief (under 4 weeks), it’s safe and effective. Ondansetron (Zofran) is another option, especially if you’re vomiting. The orally disintegrating tablets work fast - 76% of patients in one clinic reported relief within 15 to 20 minutes. But don’t use them daily unless your doctor says so. They’re meant for flare-ups, not daily maintenance.
Track Your Symptoms - It’s Not Just a Journal, It’s a Tool
Write down what you eat, when you eat it, what you drink, and how bad your nausea is on a scale of 1 to 10. Do this for just two weeks. You’ll start seeing patterns. One patient realized her nausea spiked every time she had a latte with breakfast. Another found that eating fruit on an empty stomach made things worse. A third noticed nausea disappeared when she took her injection at bedtime instead of in the morning. Patients who kept a journal for two weeks identified their personal triggers with 89% accuracy. That’s not magic. It’s data.Red Flags: When Nausea Is More Than a Side Effect
Most GLP-1 nausea fades. But if you’re vomiting more than 3 times a day for over 24 hours, can’t keep fluids down for 12 hours, or lose more than 5% of your body weight in a week - stop and call your doctor. These could be signs of gastroparesis, a rare but serious condition where the stomach stops moving food entirely. It affects about 0.5% of GLP-1 users. Early detection matters. If you’ve had nausea for more than 8 weeks without improvement, get checked.What’s Next for GLP-1 Nausea?
The future is looking better. Novo Nordisk’s oral version of semaglutide, currently in Phase 3 trials, shows 18% less nausea than the injectable form. Eli Lilly and others are testing combination therapies that pair GLP-1s with prokinetic agents - drugs that help the stomach move food along. Early results show a 52% drop in nausea without losing weight loss benefits. Big pharma is also stepping up. Novo Nordisk gives free dietitian access to most insured Wegovy patients. Eli Lilly sends new Mounjaro users free nausea kits with ginger chews and acupressure bands. The bottom line? Nausea doesn’t have to be the reason you quit. With the right approach - small meals, careful timing, slow dosing, and smart support - most people not only tolerate GLP-1 drugs, they thrive on them.How long does GLP-1 nausea usually last?
For most people, nausea starts within the first week of beginning or increasing a GLP-1 dose and lasts 4 to 8 days. About 80% of cases resolve within 8 weeks of consistent use. If nausea persists beyond 8 weeks, especially with vomiting or early fullness, it’s important to see your doctor to rule out gastroparesis.
Can I still drink coffee with my GLP-1 medication?
You can, but timing matters. Avoid drinking coffee with meals - it can worsen nausea and stomach irritation. Instead, wait at least 30 minutes after eating. Black coffee is better than sugary lattes, which are high in fat and sugar. Some people find caffeine makes nausea worse, so if you notice a pattern, try switching to herbal tea.
Is it safe to take ginger with my GLP-1 drug?
Yes, ginger is safe and often recommended. Studies show it reduces nausea by up to 62% in people on GLP-1 medications. You can take it as tea, chews, capsules, or fresh root. No known interactions exist between ginger and semaglutide, tirzepatide, or liraglutide. Just avoid excessive amounts - more than 4 grams per day - if you’re on blood thinners.
Should I take my GLP-1 injection in the morning or at night?
There’s no right or wrong time, but many people find nighttime dosing helps. When you’re asleep, your body is less sensitive to nausea signals. If you get morning nausea, try switching your injection to bedtime. One study found 63% of patients reported less nausea after making this change. Just be consistent - take it at the same time each week.
What if I miss a dose because of nausea?
If you miss a dose, take it as soon as you remember - as long as it’s within 5 days of your scheduled injection. If it’s been more than 5 days, skip the missed dose and resume your regular schedule. Don’t double up. If nausea keeps you from taking your dose regularly, talk to your doctor about slowing your titration or using an antiemetic temporarily.
Do acupressure wristbands really work for GLP-1 nausea?
Yes, in clinical studies and real-world use. A 2023 pilot study showed 80% of users experienced relief within 20 minutes of wearing the bands. They work by stimulating the P6 acupressure point on the wrist, which is proven to reduce nausea across multiple conditions. They’re non-invasive, reusable, and have no side effects. Many patients use them during the first 6 weeks of treatment and then stop once nausea improves.
Can I eat fruit on a GLP-1 medication?
Yes, but choose wisely. Low-sugar fruits like berries, green apples, and kiwi are fine in small portions. Avoid high-sugar fruits like mango, pineapple, or dried fruit, especially on an empty stomach. Fruit juice should be avoided entirely - it’s concentrated sugar and can spike nausea. Eat whole fruit with a protein or fat source - like a handful of almonds - to slow digestion and reduce stomach upset.
Is nausea worse with Mounjaro than Ozempic?
At equivalent doses, Mounjaro (tirzepatide) tends to cause slightly more nausea than Ozempic (semaglutide). At the 15 mg dose, about 35% of users report nausea compared to 44% at the 2.4 mg dose of semaglutide. But the difference isn’t huge. Both drugs cause nausea because they slow digestion. The key isn’t which drug you’re on - it’s how slowly you increase the dose and what you eat.







Jarrod Flesch
January 20, 2026 AT 20:47Barbara Mahone
January 22, 2026 AT 10:02Kelly McRainey Moore
January 24, 2026 AT 06:53Gerard Jordan
January 25, 2026 AT 07:02Stephen Rock
January 26, 2026 AT 11:44lokesh prasanth
January 27, 2026 AT 13:01MAHENDRA MEGHWAL
January 28, 2026 AT 22:20Sangeeta Isaac
January 30, 2026 AT 12:42Melanie Pearson
January 31, 2026 AT 06:48Uju Megafu
February 2, 2026 AT 02:19