Theophylline-Ciprofloxacin Interaction Calculator
Safer Antibiotic Alternatives
Imagine you’re on ciprofloxacin for a stubborn sinus infection, and you’ve been taking theophylline for years to manage your COPD. You feel fine-until suddenly, you’re nauseous, your heart is racing, and you can’t stop shaking. That’s not just bad luck. It’s a well-known, preventable medical emergency caused by one of the most dangerous drug interactions in modern medicine.
Why Ciprofloxacin and Theophylline Don’t Mix
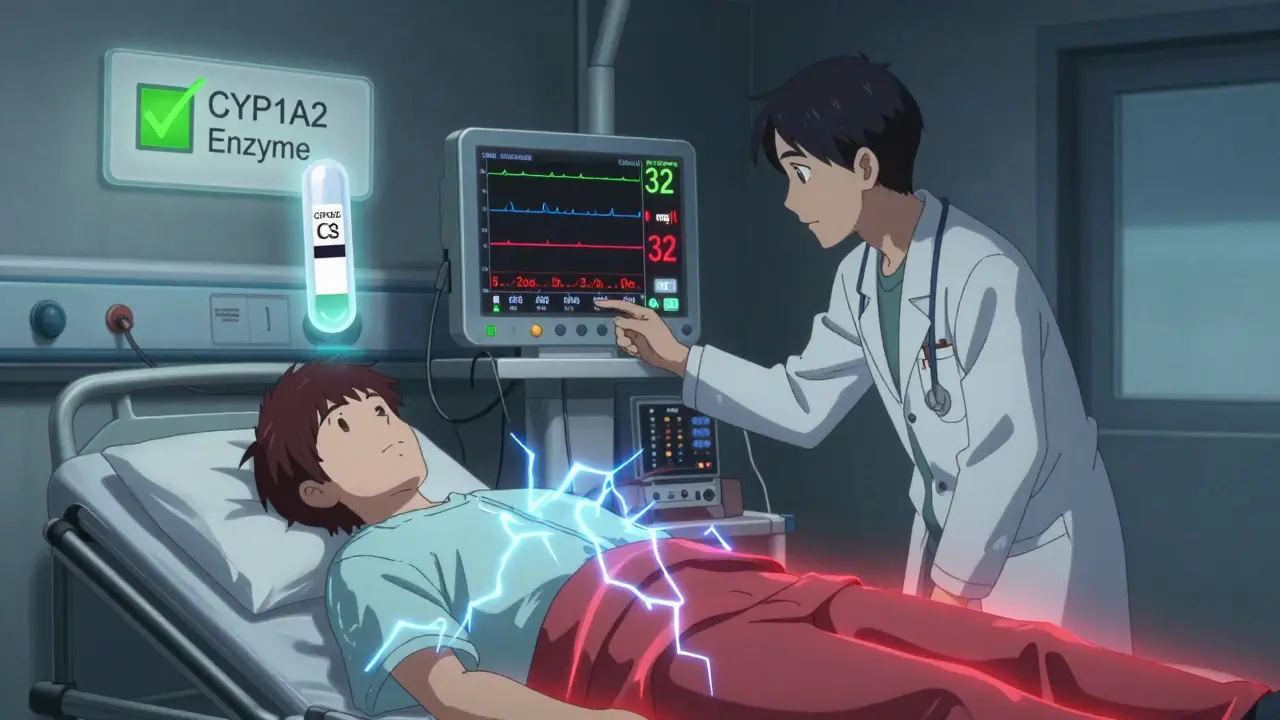
Ciprofloxacin is a powerful antibiotic, often prescribed for urinary tract infections, pneumonia, or bronchitis. Theophylline, on the other hand, is an older but still used bronchodilator for asthma and COPD. Both are common. But when taken together, they create a perfect storm.The problem lies in how your body breaks down theophylline. It relies almost entirely on an enzyme called CYP1A2. Ciprofloxacin shuts down this enzyme like flipping a switch. Without it, theophylline doesn’t get cleared from your bloodstream. Instead, it builds up-fast.
Normal theophylline levels stay between 10 and 20 mg/L. That’s a narrow window. Go above 20 mg/L, and you start seeing side effects: nausea, vomiting, headaches, jitteriness. At 25-30 mg/L, your heart can go into dangerous rhythms. Above 30 mg/L? Seizures. And yes, people have had grand mal seizures from this combo, even if they’d never had one before.
The Numbers Don’t Lie
This isn’t theoretical. A 2011 study of over 77,000 older adults in Ontario found that people taking ciprofloxacin while on theophylline were almost twice as likely to be hospitalized for toxicity. That’s not a small risk. That’s a major red flag.Compare that to other antibiotics. Levofloxacin? No big change in theophylline levels. Amoxicillin? None. Azithromycin? Safe. Trimethoprim-sulfamethoxazole? No problem. But ciprofloxacin? It’s the outlier. And it’s not just older people-though they’re at higher risk. Anyone on theophylline is vulnerable.
Studies show ciprofloxacin can increase theophylline levels by 40% to 80%. That means if you’re taking 300 mg of theophylline daily, your body might start acting like you’re taking 500 mg or more. And because theophylline has such a narrow safety margin, that’s enough to cross into toxic territory.
Who’s Most at Risk?
Elderly patients are hit hardest. Their livers don’t clear drugs as well. A 2015 meta-analysis found that in people over 65, ciprofloxacin reduces theophylline clearance by 45%-compared to 35% in younger adults. That means dose reductions need to be bigger, and monitoring needs to be tighter.But it’s not just age. People with liver disease, smokers (who metabolize theophylline faster), or those with certain genetic variants in the CYP1A2 gene are also at higher risk. One ongoing study at the University of Toronto found that patients with the CYP1A2*1F gene variant see a 65% greater drop in theophylline clearance when taking ciprofloxacin. That’s a huge difference.
What Happens When You Ignore the Warning
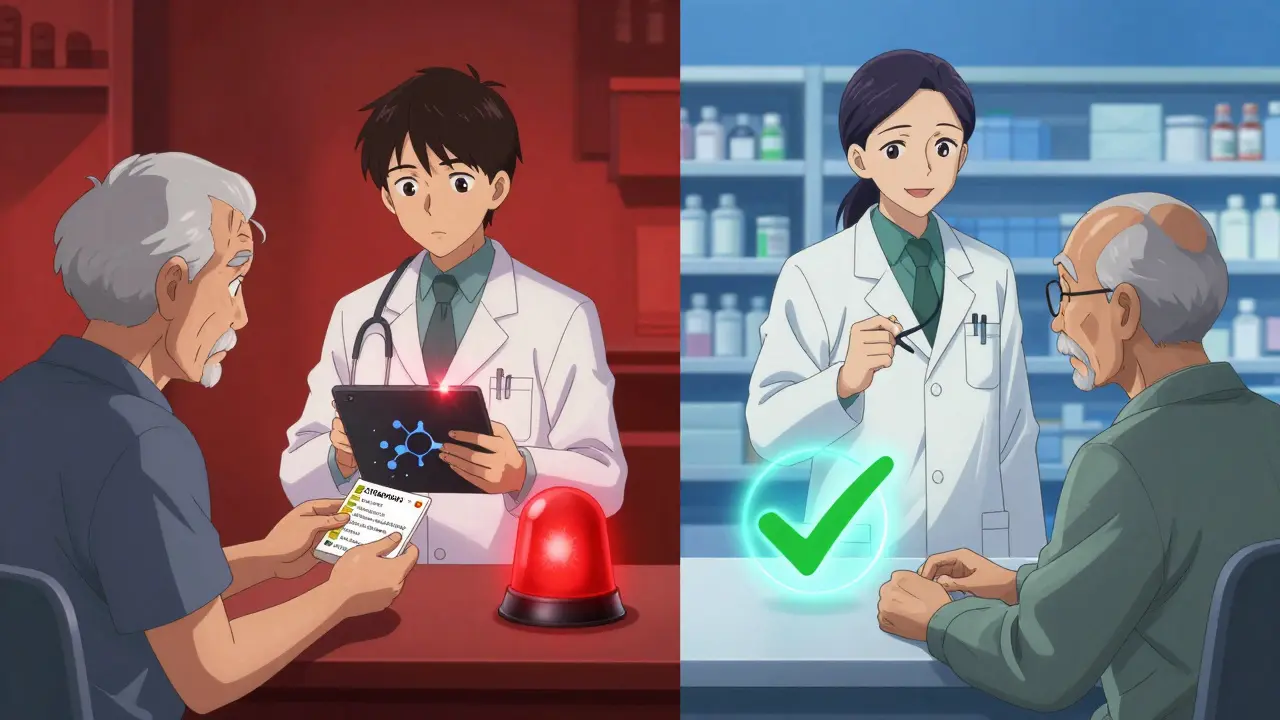
The FDA added a black box warning to ciprofloxacin labels in 1994. That’s the strongest warning they give. It says: monitor theophylline levels and reduce the dose by at least 33% if you must use both.Yet, a 2018 study found that over 12% of older adults still got ciprofloxacin while on theophylline. Why? Doctors often override electronic alerts because they think the infection is urgent, or they assume the patient “tolerated it before.” But tolerance doesn’t mean safety. The same patient who didn’t get sick last time might be dehydrated this time, or have a new kidney issue, or be on a higher dose of theophylline. The risk changes.
And it’s not just one hospitalization. In the U.S., an estimated 4,200 hospitalizations every year are caused by this interaction. Around 9,300 adverse events in Medicare patients alone are directly linked to ciprofloxacin and theophylline being used together. That’s thousands of people who could have stayed home-if someone had checked the drug interaction.
What Should You Do Instead?
If you’re on theophylline and need an antibiotic, don’t panic. But do ask: Is ciprofloxacin really the best choice?Here are safer alternatives:
- Levofloxacin - Causes only a 10-15% rise in theophylline levels. Often a good substitute.
- Moxifloxacin - Minimal effect on CYP1A2. Safe for most patients.
- Amoxicillin-clavulanate - No known interaction. Great for respiratory infections.
- Azithromycin - Doesn’t affect theophylline metabolism. Commonly used for bronchitis.
If no alternatives exist and ciprofloxacin is absolutely necessary, follow these steps:
- Check your theophylline blood level before starting ciprofloxacin.
- Reduce your theophylline dose by 30-50% right away.
- Check your level again within 24-48 hours of starting ciprofloxacin.
- Watch for early signs: nausea, vomiting, fast heartbeat, tremors, trouble sleeping.
- Stop both drugs and call your doctor immediately if you feel confused, dizzy, or have chest pain.
Why This Keeps Happening
You’d think after 35+ years of documented cases, this interaction would be a no-brainer. But here’s the reality: many clinicians still don’t know the details. A 2017 study found that nearly 70% of electronic alerts warning about this interaction were ignored. Why? Time pressure. Assumptions. Overconfidence.It’s also easy to forget. Theophylline isn’t used as much as it once was. Many younger doctors have never seen a patient on it. But it’s still out there-especially in older adults with long-standing COPD. And when they get sick, ciprofloxacin is often the go-to antibiotic because it’s broad-spectrum and convenient.
That convenience can kill.
What’s Next?
Research is moving toward personalized medicine. Genetic testing for CYP1A2 variants could soon tell doctors whether you’re at high risk before they even prescribe ciprofloxacin. But until then, the old rules still apply: check levels, reduce doses, pick safer antibiotics.This isn’t about fear. It’s about awareness. One simple question-“Is this patient on theophylline?”-could prevent a seizure, a trip to the ICU, or even death.
Don’t assume. Don’t rely on memory. Don’t trust that “it was fine before.” Double-check. Ask. Verify. Because in this case, the difference between safety and disaster is a single blood test and a few changes to a prescription.
Can I take ciprofloxacin if I’m on theophylline?
It’s not recommended. Ciprofloxacin can cause dangerous buildup of theophylline in your blood, leading to seizures, heart rhythm problems, or death. If you must take both, your theophylline dose needs to be reduced by 30-50% and your blood levels must be checked within 24-48 hours. Safer antibiotics like levofloxacin, azithromycin, or amoxicillin-clavulanate are preferred.
What are the first signs of theophylline toxicity?
Early signs include nausea, vomiting, headache, restlessness, tremors, and a fast or irregular heartbeat. These can appear within hours of taking ciprofloxacin. If you experience any of these while on both drugs, contact your doctor immediately. Do not wait for seizures or chest pain-they mean you’re already in danger.
Does levofloxacin have the same interaction?
No. Levofloxacin has minimal effect on the CYP1A2 enzyme. Studies show it increases theophylline levels by only 10-15%, which is usually not clinically significant. It’s considered a safe alternative to ciprofloxacin for patients on theophylline.
How long does the interaction last?
The interaction lasts as long as ciprofloxacin is in your system. It takes about 2-3 days for ciprofloxacin to fully clear after your last dose. Theophylline levels should be monitored for at least 5-7 days after stopping ciprofloxacin, since levels can still drop slowly. Never adjust your theophylline dose without checking blood levels first.
Why isn’t this interaction more widely known?
Many clinicians assume theophylline is no longer used, or they forget the interaction because it’s not common in younger patients. Electronic alerts are often overridden because of perceived urgency or past tolerance. But this interaction is well-documented since 1987, with thousands of cases reported. Awareness gaps persist due to outdated prescribing habits and lack of training on older medications.
Can I take theophylline again after stopping ciprofloxacin?
Yes, but only after your theophylline levels are checked and your dose is readjusted. Once ciprofloxacin is cleared, your body will start metabolizing theophylline normally again. If you go back to your original dose too soon, you risk toxicity. Always consult your doctor before restarting theophylline after stopping ciprofloxacin.






lisa Bajram
January 9, 2026 AT 08:17Yikes. I had no idea this combo could be this dangerous. My grandma’s on theophylline and her doctor just prescribed her cipro last month-thank god I caught this before she took it. I’m printing this out and handing it to her PCP tomorrow. This is the kind of info that saves lives.
Bradford Beardall
January 9, 2026 AT 13:10Same. I’m a respiratory therapist and we still see this happen. One guy came in with a seizure because his doc didn’t adjust his theophylline. He was 72, had COPD for 30 years, and they just assumed he’d be fine. The system’s broken when a black box warning gets ignored 70% of the time.
Jay Amparo
January 11, 2026 AT 12:54As someone from India where theophylline is still widely used because it’s cheap and accessible, I’ve seen this play out too. Doctors here don’t always have time to check interactions. We rely on pharmacists to catch these things-but even they’re stretched thin. This post is a wake-up call for global practice, not just the US.
Aurora Memo
January 11, 2026 AT 16:59I appreciate how thorough this is. I’ve had patients panic when I tell them to stop a med, but this breakdown makes it easier to explain why we need to switch. I’m saving this as a reference for my next clinic day.
Ian Cheung
January 11, 2026 AT 22:18My uncle died from this exact interaction 10 years ago. No one told him. He was on theophylline for 20 years. Got cipro for a sinus infection. Thought he was just getting worse from the bug. Ended up in cardiac arrest. No one even connected the dots until it was too late. This needs to be taught in med school like it’s a law.
Jake Nunez
January 13, 2026 AT 10:16Levofloxacin is the way to go. I’ve used it for years as a substitute and never had an issue. Cipro’s not worth the risk when there are safer options. Why are we still using the dangerous one?
Ashlee Montgomery
January 15, 2026 AT 07:44It’s wild how one enzyme can be the difference between life and death. CYP1A2 isn’t even a name most people know, but it’s literally keeping people alive. We treat drugs like they’re interchangeable when they’re actually this fragile. It’s not just about prescriptions-it’s about how we think about biology.
Christine Milne
January 16, 2026 AT 12:48While I appreciate the sentiment, this post exhibits a concerning trend of alarmism. Theophylline is an obsolete medication, and its continued use is medically indefensible in the 21st century. Modern alternatives such as LABAs and LAMAs are superior in safety, efficacy, and compliance. The real issue is not ciprofloxacin-it is the persistence of archaic pharmacotherapy in the face of evidence-based guidelines. This interaction is a symptom of a larger systemic failure in clinical inertia.
Michael Marchio
January 17, 2026 AT 20:07Let’s be real-this isn’t even close to the worst drug interaction out there. You’ve got warfarin and antibiotics, statins and grapefruit juice, SSRIs and triptans… this one’s just the latest flavor of the month. And yet, people act like this is some groundbreaking revelation. The truth? Most clinicians know this. They just don’t care enough to change. Or worse-they’re too lazy to look it up. This post reads like a medical school lecture someone copied and pasted. I’ve seen it before. And I’ve seen patients die from things far more preventable than this.
Lisa Cozad
January 18, 2026 AT 21:22My mom’s on theophylline and just got cipro last week. I’m calling her doctor right now. Thank you for writing this. I didn’t know what to look for-but now I know to watch for tremors and nausea. I’m so glad I found this before something happened.
Jake Kelly
January 20, 2026 AT 02:26Just want to say thanks for the clear, calm breakdown. No drama, no fearmongering-just facts and actionable steps. This is the kind of post that makes me believe there’s still hope for better care.