Every year, thousands of patients in the U.S. are harmed or killed by medication errors - many of them avoidable. A 2024 study from the Pharmacy Workflow and Safety Network found that nearly 1 in 5 prescriptions processed in high-volume community pharmacies still contain at least one preventable error. These aren’t just typos or misreads. They’re wrong doses, allergic reactions missed, drug interactions overlooked, and IV bags compounded with the wrong concentration. The problem isn’t that pharmacists are careless. It’s that the old way of doing things - paper scripts, manual counting, handwritten labels - was never built for the volume and complexity of modern medicine.
How Pharmacy Workflow Systems Work
Modern pharmacy workflow systems aren’t just fancy computers. They’re integrated networks of hardware, software, and protocols designed to catch mistakes before they reach the patient. At their core, they turn a chaotic, human-dependent process into a controlled, step-by-step sequence. Here’s how it typically flows:- A digital prescription arrives from a doctor’s EHR system, automatically routed to the pharmacy’s system.
- The software checks the patient’s profile for allergies, drug interactions, duplicate therapies, and dosage limits - all in under 2 seconds.
- If something’s off, the system flags it and alerts the pharmacist before any physical handling begins.
- The pharmacist reviews the alert, approves or adjusts the order, then sends it to the next stage.
- Robot arms or automated counting machines pull the exact number of pills from the correct bottle, verified by barcode scanning at every step.
- Labels are printed with patient-specific details, including warnings and instructions, generated from the system, not typed manually.
- Before the medication leaves the pharmacy, a final scan confirms the right drug, right dose, right patient, right route - every time.
This isn’t science fiction. It’s standard in hospitals like Johns Hopkins and major chains like CVS and Walgreens. The key difference? Every step is documented, tracked, and auditable. No more guessing if a tech counted correctly. The system knows.
Key Technologies Behind Error Prevention
Several technologies work together to make this possible:- Barcode Verification: Every pill bottle, IV bag, and patient wristband has a unique barcode. Scanning at each stage confirms match - no exceptions.
- Automated Dispensing Cabinets (ADCs): Devices like BD Pyxis™ store medications securely and only release them when the right prescription and user credentials are scanned. They track inventory in real time and alert staff when drugs are low or expiring.
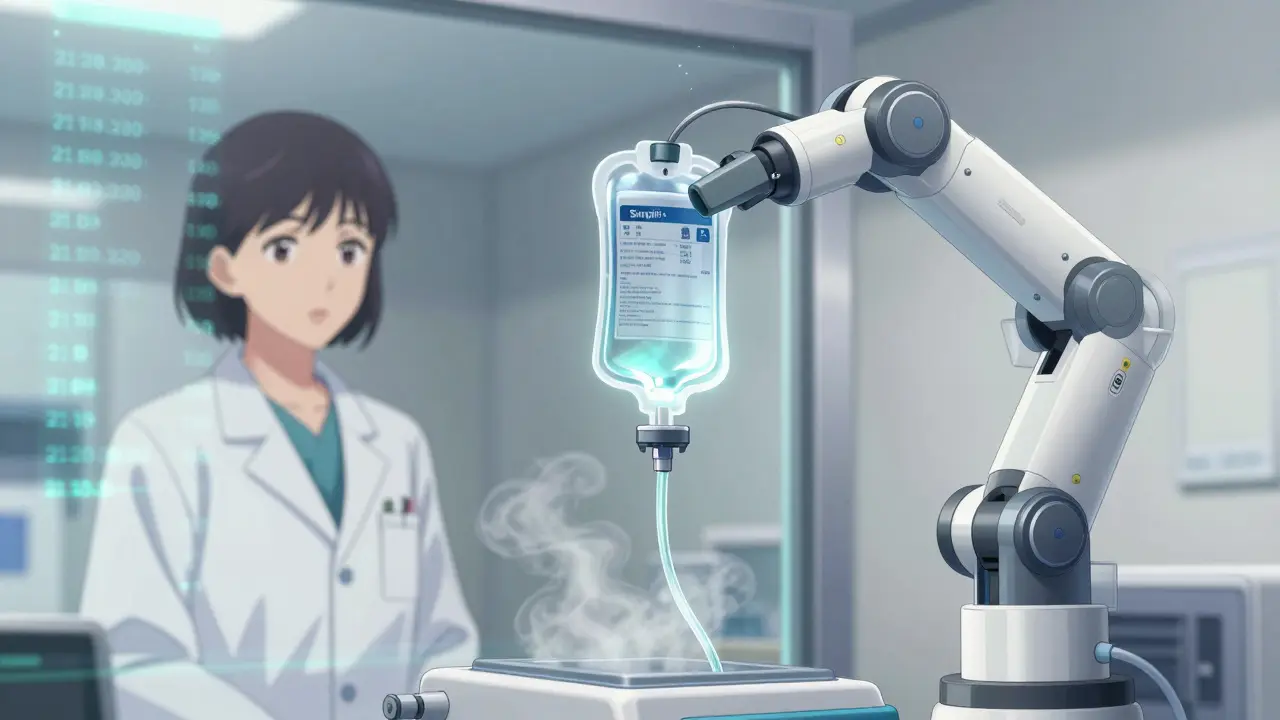
- IV Compounding Robots: Machines like the Simplifi+ IV Workflow Management system from Wolters Kluwer measure, mix, and label sterile IV solutions with precision. Human hands never touch the final product, reducing contamination and dosing errors.
- Electronic Health Record (EHR) Integration: Through HL7 interfaces, pharmacy systems pull real-time data from hospital records - lab results, kidney function, recent prescriptions - to make smarter decisions.
- Workflow Management Software: Tools like KanBo and Cflow help assign tasks, track progress, and flag delays. A prescription stuck in “verification” for over 30 minutes? The system nudges the right person.
These aren’t standalone gadgets. They’re linked. When a robot compounds an IV, it logs the batch number and ingredients into the EHR. When a pharmacist overrides a warning, the system asks why and stores the reason. Every action leaves a trail.
What Systems Actually Prevent
Let’s be specific. What kinds of errors do these systems stop?- Wrong patient: A barcode scan confirms the patient’s ID matches the prescription - no more giving insulin to the wrong person.
- Wrong drug: If a pharmacist reaches for vancomycin instead of verapamil, the barcode won’t match. The system won’t let it proceed.
- Wrong dose: A 10x overdose? The system compares the order to standard dosing guidelines and flags it instantly.
- Drug interactions: If a patient is on warfarin and the script adds amiodarone, the system shows the risk of fatal bleeding and suggests alternatives.
- Expired or recalled drugs: Inventory systems auto-block expired stock. No manual checking needed.
- Missing documentation: If a prescriber didn’t sign the e-script, the system won’t allow dispensing.
A 2023 study in the Journal of the American Pharmacists Association found that hospitals using full workflow automation saw a 14x increase in error detection compared to manual systems. And the errors they caught? 92% were stopped before reaching the patient.
Comparing Leading Systems
Not all pharmacy workflow systems are built the same. Here’s how the major players stack up:| System | Best For | Key Feature | Integration | Cost Range (Annual) |
|---|---|---|---|---|
| BD Pyxis™ | Hospitals, ADCs | Secure automated dispensing with real-time inventory | HL7, Epic, Cerner | $80,000-$180,000 |
| Simplifi+ IV Workflow Management | IV compounding centers | Robot-assisted sterile compounding with compliance tracking | HL7, USP <797>/<800> audit logs | $120,000-$250,000 |
| Cflow | Community pharmacies | Cloud-based templates for dispensing, refill, and counseling workflows | Most EHRs, RxHub | $50,000-$120,000 |
| KanBo | Workflow visibility & team coordination | Visual task boards, card relations, deadline alerts | APIs for custom integrations | $30,000-$90,000 |
Large hospitals often use Pyxis and Simplifi+ together - one for storage and dispensing, the other for compounding. Smaller pharmacies might start with Cflow to digitize refills and reduce labeling errors. The choice depends on volume, type of meds, and budget.
Why Technology Alone Isn’t Enough
Installing a robot doesn’t fix a broken process. Many pharmacies spend $200,000 on a new system and still see errors - because they didn’t change how people work. The American Society of Health-System Pharmacists (ASHP) says successful adoption requires three things:- Workflow redesign: Don’t just plug in the machine. Map out how prescriptions move through your pharmacy. Eliminate redundant steps. Combine tasks where possible.
- Staff training: Pharmacists and techs need hands-on practice, not a 30-minute video. Simulate real errors during training so they know how the system responds.
- Leadership buy-in: If managers don’t enforce system use - like requiring barcode scans even when it’s “just a refill” - people will skip steps. Culture matters more than code.
A 2025 survey of 217 U.S. pharmacies showed that those who invested in both technology and process redesign reduced dispensing errors by 78%. Those who only bought the tech? Only 29% improvement.
Implementation Challenges
Switching systems isn’t easy. Most pharmacies report a 3- to 6-month transition period. Common issues:- Staff resistance: “I’ve done this for 20 years - why do I need a machine telling me what to do?”
- System glitches: Network outages, barcode scanner failures, or slow EHR syncs can halt workflow.
- Training gaps: Techs trained on one system get moved to another and get confused.
- Cost: A full enterprise system can cost more than hiring three new pharmacists.
One 340B hospital in Ohio struggled for months because their old system didn’t talk to the new one. The fix? A custom HL7 interface built by their IT team - now they track every step from order to delivery with zero manual entry.
What’s Next?
The next wave of pharmacy systems will use AI not just to catch errors, but to predict them.- Predictive inventory: Systems will forecast which drugs will run out based on seasonal trends, flu outbreaks, or supply chain delays.
- AI-powered alerts: Instead of generic warnings, the system will say, “Patient has chronic kidney disease. This dose is 3x higher than safe for their GFR.”
- Telehealth integration: A patient gets a prescription via video visit - the system auto-checks their home meds, insurance coverage, and delivery logistics before the script even reaches the pharmacy.
Regulations are catching up too. USP <797> and <800> standards now require digital audit trails for sterile compounding. HIPAA compliance is non-negotiable. Cloud-based systems with 99.9% uptime are becoming the norm, not the luxury.
The goal isn’t to replace pharmacists. It’s to free them from repetitive, high-risk tasks so they can do what humans do best - talk to patients, spot subtle signs of misuse, and make judgment calls when the system says “maybe.”
Final Thoughts
Medication errors are preventable. Not because we’re better at counting pills. But because we stopped relying on memory, handwriting, and hope. Pharmacy workflow systems are the most effective tool we have to make sure the right drug gets to the right person, at the right time, every single time. They don’t eliminate human judgment - they enhance it. And in a field where one mistake can cost a life, that’s not just efficient. It’s essential.How do barcode systems prevent medication errors in pharmacies?
Barcode systems scan every item in the medication chain - from the drug bottle to the patient’s wristband. At each step, the system confirms the drug, dose, patient, and route match the electronic prescription. If there’s a mismatch - say, the wrong pill is picked - the system blocks the next step and alerts the pharmacist. This eliminates human misreads, especially with look-alike or sound-alike drugs like hydralazine and hydroxyzine.
Are pharmacy workflow systems only for hospitals?
No. While hospitals use advanced systems like Pyxis and Simplifi+ for IV compounding and high-volume dispensing, community pharmacies benefit too. Systems like Cflow and KanBo help small pharmacies automate refills, reduce labeling errors, track inventory, and improve patient counseling workflows. Even a single pharmacy can cut dispensing errors by 40% with basic digital workflow tools.
What’s the biggest mistake pharmacies make when adopting new systems?
The biggest mistake is thinking the technology fixes everything. Many pharmacies buy a robot or software but keep their old workflows - like letting techs bypass scans during busy hours. Success comes from redesigning the process around the system, training staff thoroughly, and enforcing compliance. Technology is the tool; people and process are the engine.
How much do pharmacy workflow systems cost?
Costs vary widely. Basic cloud-based systems for small pharmacies start around $30,000-$50,000 per year. Mid-sized systems with inventory and e-prescribing tools cost $70,000-$120,000. Full hospital-grade systems with robotics and IV compounding can reach $200,000-$250,000 annually. Most include software updates and support, but implementation and training are extra.
Do these systems reduce pharmacist workload?
They reduce repetitive, high-risk tasks - like counting pills or checking for interactions - but not overall workload. Pharmacists shift from manual checking to supervising, interpreting alerts, and talking to patients. Many report feeling less stressed because they’re not constantly second-guessing themselves. The work becomes more clinical and less mechanical.
How do pharmacy systems handle drug shortages?
Modern inventory modules track expiration dates and stock levels in real time. When a drug runs low, the system flags it and suggests alternatives based on clinical equivalence. Some systems even auto-alert suppliers or notify prescribers if a substitution is needed. This prevents delays and ensures patients get safe, effective replacements without manual searching.
Can pharmacy workflow systems integrate with telehealth platforms?
Yes, newer systems are designed to connect with telehealth platforms. When a virtual visit results in a prescription, the system pulls the patient’s full history - including allergies, current meds, and lab results - before the script even hits the pharmacy. Some even auto-schedule delivery or notify the patient about pickup times, reducing no-shows and improving adherence.








Nancy Nino
February 2, 2026 AT 01:46Wow. So we’ve finally admitted that humans are terrible at counting pills and reading handwriting. Took long enough. I’m just glad we’re moving from ‘hope for the best’ to ‘verify every damn step.’
Deep Rank
February 2, 2026 AT 17:42ok so i read this whole thing and like… i think its great but also… why are we spending 250k on a robot to mix ivs when we could just hire more pharma techs who actually care? like i get the tech but dont we just be replacing humans with machines that still need humans to fix them? also the word ‘compliance’ is used 17 times and i think its a red flag lol
Ishmael brown
February 4, 2026 AT 08:30🤖💥 I’m not saying the robots are evil… but I DID see one cry in a hospital hallway last week. It was holding a mislabeled vial. And it… sighed. 😢
Look. I get it. Tech is cool. But when your IV bot starts writing poetry about ‘the loneliness of sterile environments’… we’ve gone too far. #PharmaRobotApocalypse
Aditya Gupta
February 5, 2026 AT 01:14Big win for patient safety. But the real win? Pharmacists getting to talk to patients again instead of playing human barcode scanners. That’s the future.
Start small. Cflow for refills. Train your team. Then scale. No need to buy a $200k robot on day one.
Jamie Allan Brown
February 6, 2026 AT 10:50This is a thoughtful, well-structured breakdown. I appreciate how you emphasize that technology is an enabler, not a replacement. The cultural shift-training, workflow redesign, leadership buy-in-is what truly makes these systems work. Too often, we treat tech as a magic bullet. It’s not. It’s a tool. And tools need skilled hands to be effective.
Lisa Rodriguez
February 7, 2026 AT 11:19Love this. My cousin’s a pharmacist in Ohio and she said the new system cut her error-checking time in half. Now she actually has time to ask patients how they’re feeling, not just if they’re taking their meds. That’s the real win.
Also the part about AI predicting errors? That’s next level. Imagine it saying ‘this patient’s kidneys are declining, this dose is risky’ instead of just flashing a warning. Game changer.
Nicki Aries
February 9, 2026 AT 09:38It’s astonishing-truly astonishing-that we ever allowed a system where a human being, under pressure, with fatigue, and with a brain that forgets things, was entrusted with the responsibility of counting out 120 pills by hand… and expecting perfection. The fact that this was ever acceptable is a moral failure. We are not engineers. We are not robots. We are flawed. And now, finally, we are using machines to protect us from ourselves. I am grateful.
Ed Di Cristofaro
February 10, 2026 AT 16:32So let me get this straight… we spent millions on robots so pharmacists don’t have to count pills… but they still get paid like they’re doing brain surgery? Bro. Just pay them more. No robot needed. They’re overworked, underpaid, and now they’re babysitting machines too? What a joke.
Lilliana Lowe
February 12, 2026 AT 13:44The article contains several grammatical inconsistencies, notably the inconsistent use of em-dashes and the misplacement of commas in compound sentences. Furthermore, the term 'Simplifi+' is incorrectly capitalized-it should be 'Simplifi+' (lowercase 'i') per the manufacturer's official branding guidelines. Additionally, the reference to 'USP ' is incomplete; it should specify 'USP <797>' or 'USP <800>' depending on context. While the overall message is commendable, precision in technical documentation is non-negotiable.