Hypoglycemia Risk Calculator
This tool calculates your risk of hidden hypoglycemia when taking insulin and beta-blockers. Beta-blockers can mask critical warning signs of low blood sugar. Enter your details to understand your personal risk level and safety steps.
Why Insulin and Beta-Blockers Together Can Be Dangerous
If you’re taking insulin for diabetes and also a beta-blocker for high blood pressure or heart disease, you’re in a high-risk group-and most people don’t realize it. Beta-blockers, which are commonly prescribed after a heart attack or for chronic hypertension, can hide the warning signs of low blood sugar. This isn’t just a minor inconvenience. It’s a life-threatening combo.
When your blood sugar drops too low, your body normally sends out alarms: your heart races, your hands shake, you break out in a cold sweat. These are your body’s way of saying, “Eat something now.” But beta-blockers block those signals. The racing heart? Gone. The trembling? Masked. What’s left? Silence. And that silence can kill.
Studies show that about 40% of people with type 1 diabetes develop hypoglycemia unawareness over time. That means they no longer feel the early signs of low blood sugar. Add a beta-blocker into the mix, and that risk jumps even higher. In hospitals, where insulin and beta-blockers are often given together, nearly a quarter of diabetic patients are on both drugs. And 68% of dangerous low-blood-sugar events in these patients happen within the first 24 hours.
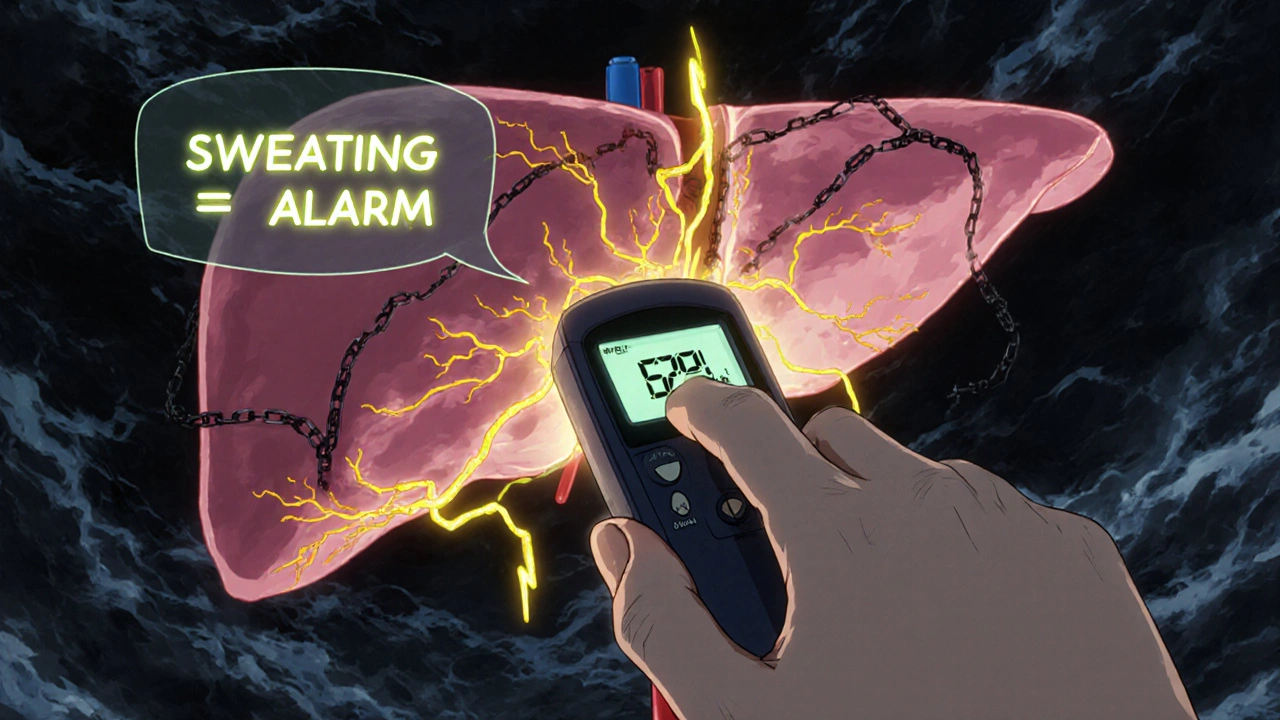
How Beta-Blockers Silence Your Body’s Warning System
Beta-blockers work by blocking adrenaline-specifically, the effects of epinephrine and norepinephrine on your heart and blood vessels. That’s good for lowering blood pressure and reducing heart strain. But it’s bad news when your blood sugar crashes.
Adrenaline is one of your body’s main tools for fighting low blood sugar. It triggers:
- Tachycardia (fast heartbeat)
- Tremors (shaky hands)
- Anxiety or nervousness
- Palpitations
These are all classic hypoglycemia symptoms. Beta-blockers shut them down. That’s why people on these drugs often don’t realize they’re going low until it’s too late-until they’re confused, dizzy, or unconscious.
But here’s the critical detail most people miss: sweating is still there. Unlike the other symptoms, sweating is controlled by a different system-acetylcholine, not adrenaline. So if you’re on a beta-blocker and you start sweating for no reason, especially if you haven’t been active or it’s not hot, that’s your body’s last warning. Don’t ignore it. Check your blood sugar immediately.
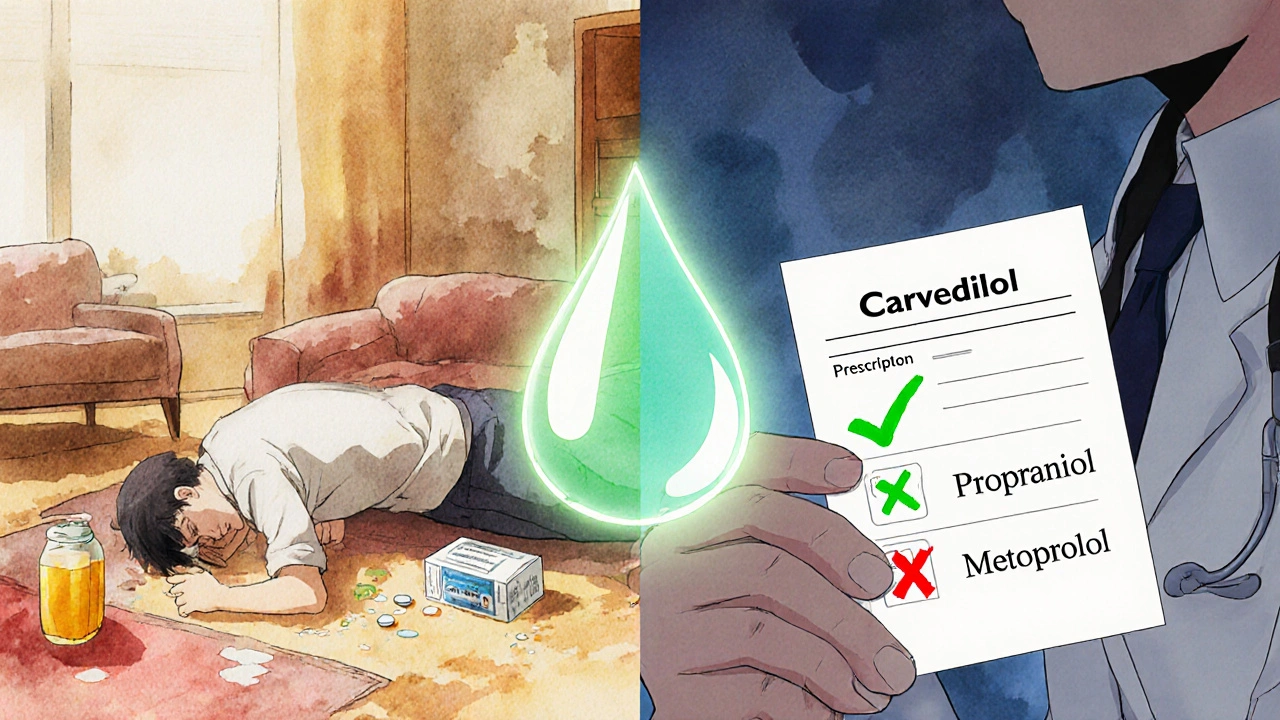
Not All Beta-Blockers Are the Same
There’s a big difference between types of beta-blockers. Some are selective. Some aren’t. And that matters a lot when you’re on insulin.
Non-selective beta-blockers (like propranolol) block both beta-1 and beta-2 receptors. They’re more likely to completely mask hypoglycemia symptoms. They also interfere with your liver’s ability to release stored glucose when your blood sugar drops. That means your body can’t correct the low on its own.
Selective beta-blockers (like metoprolol or atenolol) mainly target the heart (beta-1 receptors). They’re less likely to cause full-blown unawareness-but they still raise your risk. One study found that patients on selective beta-blockers had 2.3 times higher odds of severe hypoglycemia compared to those not taking them.
Then there’s carvedilol. It’s different. It blocks beta receptors, but also alpha receptors. That gives it a unique profile. Research shows carvedilol is less likely to cause hypoglycemia unawareness than metoprolol. In fact, one study found that patients on carvedilol had a 17% lower chance of severe low blood sugar events than those on metoprolol. It also doesn’t suppress the liver’s glucose release as much. For people with diabetes on insulin, carvedilol is increasingly the preferred choice.
What Happens When Your Body Can’t Fix Low Blood Sugar
It’s not just about missing the warning signs. Beta-blockers also stop your body from fixing the problem.
When your blood sugar drops, your liver should release stored glucose (glycogen) to bring it back up. That process is controlled by beta-2 receptors. Beta-blockers, especially non-selective ones, block those receptors. So your liver stays quiet. Your muscles can’t release glucose either. Your body is stuck in low gear.
At the same time, your pancreas may stop releasing glucagon-the hormone that tells your liver to make more glucose. Beta-blockers can blunt that response too. So you’re not just missing the alarm. You’re also disabling the rescue team.
This dual failure-masked symptoms + no recovery-is why hypoglycemia on beta-blockers is so dangerous. It’s not just low blood sugar. It’s low blood sugar with no escape route.
Who’s at the Highest Risk?
Not everyone on insulin and beta-blockers will have a problem. But some groups are at much higher risk:
- People with type 1 diabetes (especially those with long-standing disease)
- Those who’ve had previous episodes of severe hypoglycemia
- Patients with hypoglycemia unawareness already diagnosed
- Older adults (over 65)
- People with kidney disease (slower drug clearance)
- Those recently hospitalized or starting a new beta-blocker
The first 24 to 48 hours after starting a beta-blocker are the most dangerous. That’s when your body is still adjusting, and your hypoglycemia awareness is at its lowest. Hospital records show that most life-threatening lows happen during this window.
Even if you’ve been stable for years, adding a beta-blocker can reset your body’s warning system. You might think you know your lows. But you don’t-not anymore.
What You Should Do Right Now
If you’re on insulin and a beta-blocker, here’s what you need to do immediately:
- Check your blood sugar more often. At least every 4 hours during the day. If you’re in the hospital, check every 2 hours. Don’t wait for symptoms.
- Learn to recognize sweating as your new warning sign. If you’re sweating without exertion, heat, or stress-test your blood sugar. Right now.
- Ask your doctor if you can switch to carvedilol. If you’re on propranolol, atenolol, or metoprolol, ask if carvedilol is an option. It’s safer for your blood sugar.
- Get a continuous glucose monitor (CGM). CGMs have reduced severe hypoglycemia by 42% in people on beta-blockers. They give you real-time alerts-even when your body doesn’t.
- Never skip meals or delay eating. Beta-blockers make your body less able to compensate for missed meals. Even a small delay can trigger a low.
Keep fast-acting glucose (glucose tablets, juice, candy) with you at all times. And tell someone close to you-your partner, your child, your coworker-what to do if you pass out. They need to know to give you glucagon or call 999.
What Doctors Are Doing Differently Now
Guidelines have changed. The American Diabetes Association, the American Heart Association, and the European Society of Cardiology all agree: beta-blockers are still essential for heart protection in diabetic patients. But they must be used smarter.
Here’s what’s now standard in hospitals and clinics:
- Carvedilol is the first-choice beta-blocker for diabetic patients
- Non-selective beta-blockers like propranolol are avoided in patients with hypoglycemia unawareness
- CGM use is strongly recommended for anyone on insulin and beta-blockers
- Patients get formal education on sweating as the only reliable symptom
- Glucose checks are built into hospital protocols-every 2-4 hours
Quality improvement programs that followed these steps cut beta-blocker-related hypoglycemia complications by 35% in just two years.
What About Long-Term Risk?
You might wonder: “If I’ve been on this combo for years and never had a problem, am I safe?”
Some studies say yes. The ADVANCE trial followed 11,000 diabetic patients for five years and found no difference in severe hypoglycemia rates between those on atenolol and those on placebo. That suggests that in stable, outpatient settings, the risk might be lower.
But other data tells a different story. Dungan’s research showed that people on selective beta-blockers had a 28% higher risk of dying from hypoglycemia than those not taking them. And those deaths often happen suddenly-no warning, no time to react.
The truth? The risk isn’t the same for everyone. It’s higher in the hospital, higher in older adults, higher if you’ve had lows before. You can’t assume you’re safe just because you’ve been fine so far.
What’s Next? Personalized Medicine and New Treatments
Researchers are now looking for ways to predict who’s most at risk. The 2023 DIAMOND trial is testing genetic markers that might tell doctors which patients are more likely to develop hypoglycemia unawareness when on beta-blockers.
There’s also early research into drugs that can restore hypoglycemia awareness. Things like methylxanthines (found in caffeine), alanine supplements, and even opioid blockers have shown promise in small studies. But these aren’t ready for routine use yet.
For now, the best tools are simple: better drug choices, better monitoring, better education. The goal isn’t to stop beta-blockers. It’s to use them safely.
Final Takeaway: Don’t Panic. Be Prepared.
This isn’t about avoiding beta-blockers. It’s about using them wisely. If you have diabetes and take insulin, beta-blockers can still save your life from heart disease. But they can also sneak up on you when your blood sugar drops.
The key is awareness. Know your body. Know your meds. Know the one warning sign that still works-sweating. Check your glucose often. Talk to your doctor about carvedilol. Get a CGM if you can.
Low blood sugar on beta-blockers doesn’t come with a warning siren. But it does come with a silent alarm. You just have to know how to listen.
Can beta-blockers cause low blood sugar on their own?
Beta-blockers don’t directly lower blood sugar like insulin does. But they can make hypoglycemia worse by blocking your body’s natural recovery system. They prevent your liver from releasing glucose and mask the warning signs, making it harder to treat low blood sugar before it becomes dangerous.
Is it safe to take carvedilol with insulin?
Yes, carvedilol is generally the safest beta-blocker for people on insulin. It has less impact on glucose recovery and is less likely to mask hypoglycemia symptoms compared to metoprolol or atenolol. Studies show a 17% lower risk of severe low blood sugar with carvedilol, making it the preferred choice in diabetic patients.
What should I do if I feel fine but my glucose monitor says I’m low?
Treat it immediately. If you’re on a beta-blocker, your body may not send warning signals-even if your blood sugar is dangerously low. Don’t wait for symptoms. Follow your hypoglycemia treatment plan: consume 15 grams of fast-acting carbs, wait 15 minutes, recheck. Repeat if needed.
Can I stop my beta-blocker if I’m worried about low blood sugar?
Never stop a beta-blocker suddenly. Doing so can trigger a heart attack, especially if you’ve had one before. If you’re concerned about hypoglycemia, talk to your doctor about switching to a safer option like carvedilol or adjusting your insulin dose. Never make changes on your own.
Do all people on insulin and beta-blockers get hypoglycemia unawareness?
No. But the risk is significantly higher. About 40% of people with type 1 diabetes develop hypoglycemia unawareness over time, and beta-blockers increase that risk. Not everyone will experience it-but if you’ve had low blood sugar before, or you’re older or have kidney disease, your risk is much higher. Assume you’re at risk until proven otherwise.
How often should I check my blood sugar if I’m on insulin and a beta-blocker?
At minimum, check every 4 hours during the day. If you’re in the hospital, check every 2 hours. If you’ve just started a beta-blocker, check even more often for the first 48 hours. Use a continuous glucose monitor (CGM) if possible-it’s the most reliable way to catch lows before they become dangerous.
Is sweating the only reliable sign of low blood sugar on beta-blockers?
Yes. Sweating is the only major autonomic warning sign that beta-blockers don’t block. It’s controlled by acetylcholine, not adrenaline. If you start sweating without reason-especially if you’re not hot or active-test your blood sugar immediately. It’s your body’s last alarm.






swatantra kumar
November 20, 2025 AT 03:28Sarah Swiatek
November 21, 2025 AT 12:56Rebecca Cosenza
November 22, 2025 AT 22:44rob lafata
November 23, 2025 AT 14:23Cinkoon Marketing
November 23, 2025 AT 19:45Pawan Jamwal
November 24, 2025 AT 03:27Lemmy Coco
November 24, 2025 AT 10:14Nick Naylor
November 24, 2025 AT 11:29Brianna Groleau
November 24, 2025 AT 12:37Matthew McCraney
November 25, 2025 AT 15:06serge jane
November 25, 2025 AT 17:01Dave Wooldridge
November 27, 2025 AT 05:32Sarah Swiatek
November 27, 2025 AT 21:47