Quick Take
- Anal itching can be a sign of lichen sclerosus, a chronic skin disease.
- Both conditions share inflammation, but lichen sclerosus also thins and whitens skin.
- Diagnosis usually involves a visual exam and sometimes a biopsy.
- First‑line treatment is high‑potency topical steroids; other options include immunosuppressants.
- Good hygiene, moisturisation, and regular follow‑up keep flare‑ups under control.
When you feel that relentless itch around the rear end, it’s easy to blame poor hygiene or a fleeting infection. Yet, for a surprising number of people, that irritation points to a deeper skin disorder called Lichen Sclerosus is a chronic inflammatory skin condition that commonly affects the genital and anal areas. Understanding how anal itching and lichen sclerosus intertwine helps you spot the problem early, get the right treatment, and stop the cycle of discomfort.
What Exactly Is Anal Itching?
Anal itching-medical term pruritus ani-is the urge to scratch the skin around the Anus is the opening at the end of the digestive tract that expels waste. It’s a symptom, not a disease, and can stem from anything that irritates the local skin: moisture, sweat, allergens, infections, or systemic conditions. The itch often feels worse at night because sweat accumulates and the skin cools, making the nerve endings more sensitive.
What Is Lichen Sclerosus?
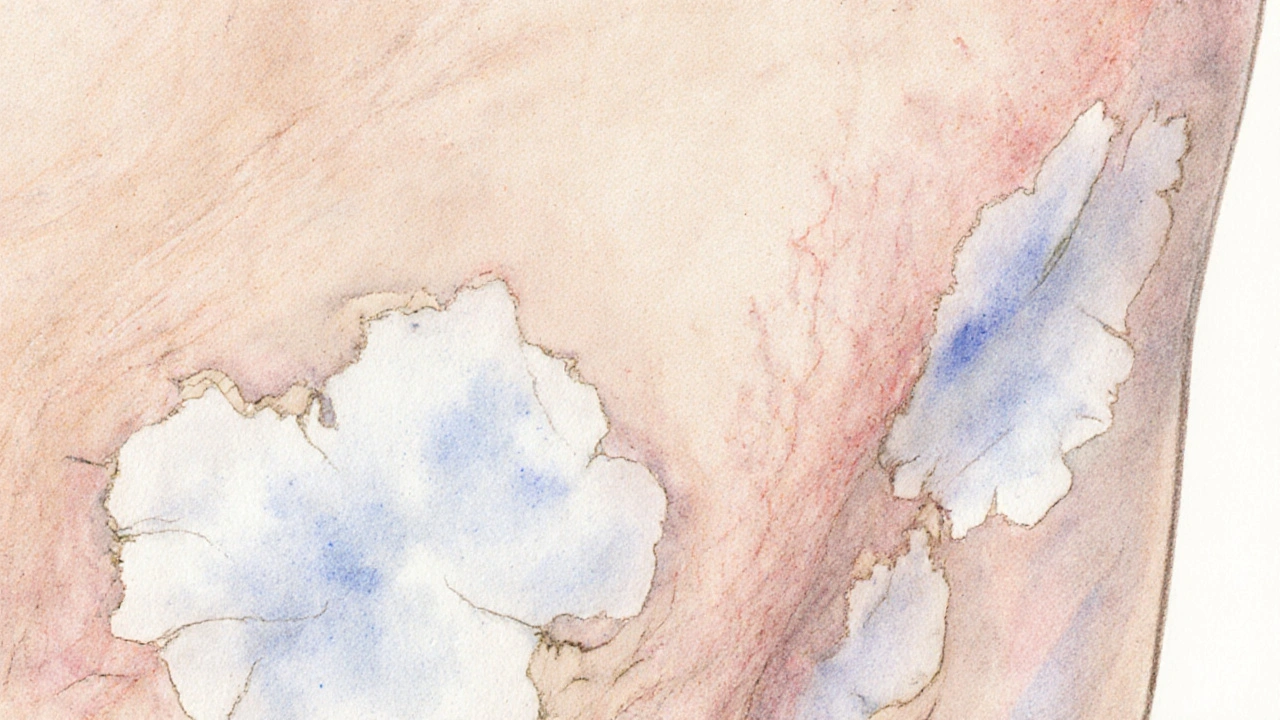
Lichen sclerosus is a misunderstood, long‑lasting skin disorder. It most often appears on the Skin is the body’s largest organ that forms a protective barrier against the environment around the genitals, but the anal region is a common site too. The disease causes thin, white patches that may crack, bleed, or scar. While anyone can develop it, women, men over 50, and post‑menopausal individuals are at higher risk.
How Anal Itching and Lichen Sclerosus Connect
The link isn’t just a coincidence-both share an underlying inflammatory process. In lichen sclerosus, the immune system mistakenly attacks the skin, releasing cytokines that trigger itching, redness, and tissue breakdown. Those same cytokines sensitize the nerve endings around the Anus, amplifying the itch sensation. Over time, persistent scratching can damage skin, creating a feedback loop where the irritation fuels more inflammation.
In many patients, the first clue that the itch isn’t just a fleeting bug bite is the appearance of white, parchment‑like plaques. If you notice these patches, especially if they’re painless yet stubborn, it’s time to think beyond simple irritation.
Recognising the Warning Signs
| Feature | Typical Anal Itching | Lichen Sclerosus |
|---|---|---|
| Onset | Sudden, often linked to diet or hygiene | Gradual, weeks to months |
| Skin appearance | Redness, possible rash, no white patches | White, atrophic plaques; may crack |
| Bleeding | Rare, usually from scratching | Common if plaques fissure |
| Location | Can be anywhere around the anus | Focused on perianal skin, often extending to genitals |
| Response to OTC creams | Usually improves quickly | Limited; may need prescription steroids |
Beyond visual cues, pay attention to duration. Itching that lingers beyond a few weeks, or that worsens despite standard moisturisers, deserves a professional eye.
Getting the Right Diagnosis
Because the symptoms overlap with other conditions-hemorrhoids, fungal infections, psoriasis-accurate diagnosis matters. Here’s what doctors typically do:
- Take a thorough history: diet, hygiene, medication, and any previous skin issues.
- Perform a visual inspection of the Anus and surrounding skin.
- If white patches are present, they may suggest Lichen Sclerosus. A gentle Biopsy is a small tissue sample examined under a microscope to confirm the diagnosis can provide certainty.
- Rule out infections with swabs or cultures when needed.
Specialist care usually comes from a dermatologist, the medical field that focuses on skin diseases. The Dermatology is the branch of medicine dealing with the skin, nails, hair and its diseases team can guide long‑term management.
Treatment Options: From First Line to Advanced Care
The cornerstone of therapy for lichen sclerosus-and for stubborn anal itching caused by it-is potent Topical Steroids are medicines applied to the skin that reduce inflammation and immune response. Common regimens include clobetasol propionate 0.05% applied once daily for 4‑6 weeks, then tapered.
When steroids aren’t enough or cause side‑effects, doctors may add Immunosuppressants are drugs that dampen the immune system’s activity, helping control chronic inflammation such as tacrolimus ointment or pimecrolimus. These are especially useful for delicate perianal skin where long‑term steroid use can thin the tissue.
In rare, refractory cases, systemic treatments-like oral retinoids or low‑dose methotrexate-might be considered, always under specialist supervision.
Practical Tips to Calm the Itch
- Keep the area dry. After bathing, pat gently with a soft towel; avoid rubbing.
- Use fragrance‑free, hypo‑allergenic moisturisers. Products containing ceramides help restore the skin barrier.
- Avoid tight underwear. Breathable cotton reduces friction and moisture buildup.
- Don’t scratch. It may feel natural, but it worsens inflammation. Keep nails trimmed and consider a cool compress to soothe.
- Watch your diet. Spicy foods, caffeine, and alcohol can aggravate itching for some people.
- Schedule regular follow‑ups. Lichen sclerosus can increase the risk of skin cancer in the affected region, so annual exams are prudent.
When you pair these lifestyle habits with medical therapy, most patients notice a dramatic drop in itch intensity within weeks.
When to Seek Immediate Help
If you experience any of the following, contact a healthcare provider promptly:
- Sudden, severe pain accompanied by bleeding.
- Rapidly spreading white patches or ulcerations.
- Signs of infection: fever, pus, foul odour.
- Any change in bowel habits that could suggest a more serious underlying condition.
Early intervention reduces the chance of permanent scarring and keeps the itch from taking over your daily life.
Frequently Asked Questions
Can anal itching be the only symptom of lichen sclerosus?
Yes. Some people notice persistent itch before any visible skin changes. If the itch lasts more than a few weeks, ask your doctor to examine the area for subtle signs of lichen sclerosus.
Is a biopsy always required?
Not always. If the classic white patches are clear and the doctor is confident, they may start treatment without a biopsy. However, a sample is recommended when the diagnosis is uncertain or if there’s suspicion of skin cancer.
Can I use over‑the‑counter creams for relief?
OTC moisturisers can soothe dryness, but they won’t treat the underlying inflammation of lichen sclerosus. Prescription Topical Steroids are needed for long‑term control.
Is lichen sclerosus contagious?
No. It’s an autoimmune‑driven condition, not an infection, so it cannot be passed to another person through skin contact.
What is the long‑term outlook?
With consistent treatment, most people achieve symptom control and avoid scarring. Regular monitoring is essential because a small percentage may develop skin cancer in the affected area.







Chris Wiseman
September 28, 2025 AT 17:37When we stare at the uncomfortable reality of chronic anal itching, we are forced to confront not just a medical condition but a philosophical paradox about the body’s silent screams; the skin, that fragile barrier, becomes a stage where immunity and irritation perform a grotesque ballet, each step echoing through the corridors of our psyche. In the grand theatre of disease, lichen sclerosus takes the role of the misunderstood antagonist, lurking beneath the surface while the unsuspecting host scrabbles for relief. It is tempting to reduce the experience to mere discomfort, yet the itch is a messenger, a reminder that the body is an ecosystem where immune dysregulation can manifest in the most intimate of ways. The inflammatory cascade, a cascade of cytokines, does not discriminate; it invades the perianal region, turning harmless skin into a parchment‑like canvas of white plaques that whisper of deeper autoimmune turmoil. One might argue that the modern world, with its obsession for quick fixes, encourages a culture of superficial treatment, slapping on over‑the‑counter creams while ignoring the underlying immunological choreography. However, scientific literature-though often cloaked in jargon-shows that high‑potency topical steroids are not just band‑aid but conductors that can restore harmony, provided they are used with diligence and respect for the skin’s delicate nature. The very act of scratching, a primal response, perpetuates a vicious feedback loop, amplifying the inflammatory signals and leading to further tissue compromise. Think of it as a conversation lost in translation; the nerves speak in fire, the immune system answers with ice, and the mind watches in bewildered silence. Moreover, the psychological burden cannot be dismissed; living with persistent itch can erode confidence, strain relationships, and foster a sense of isolation that rivals any physical symptom. The stigma attached to perianal conditions often means patients suffer in secrecy, a hidden shame that compounds the physiological distress. Yet, the medical community has made strides, recognizing that regular monitoring not only tracks disease progression but also screens for the rare yet ominous risk of malignant transformation. The emphasis on moisturisation, breathable fabrics, and dietary adjustments reflects a holistic approach, acknowledging that skin health is intertwined with lifestyle choices. In the end, acknowledging the interplay between anal itching and lichen sclerosus invites us to view the body not as a collection of isolated parts, but as an interconnected narrative where every symptom tells a story, and every treatment is a chapter toward resolution.
alan garcia petra
October 8, 2025 AT 19:17Great breakdown! Keep that positive vibe and remember, consistency with the steroid cream really makes a difference.
Allan Jovero
October 18, 2025 AT 20:57While the exposition is comprehensive, it would be prudent to underscore the necessity of obtaining a definitive histopathological diagnosis prior to instituting long‑term high‑potency corticosteroid therapy, thereby mitigating the risk of iatrogenic atrophy.
Andy V
October 28, 2025 AT 21:37Seriously, stop using “its” when you mean “it’s.” The article could use a quick edit for basic grammar.
Michelle Wigdorovitz
November 7, 2025 AT 23:17Wow, I never realized how dramatic the whole skin‑immune dance can get! It’s like the body’s own soap opera, and we’re just glued to the drama of scratching and soothing.
Arianne Gatchalian
November 18, 2025 AT 00:57I’ve been there, dealing with that relentless itch. It really helps to keep a gentle moisturizer handy and to remember you’re not alone in this.
Aly Neumeister
November 28, 2025 AT 02:37Keep it dry and avoid tight clothes
joni darmawan
December 8, 2025 AT 04:17From a philosophical standpoint, the perianal region can be seen as a microcosm of the larger human condition-where vulnerability and resilience intertwine, and where proper care reflects a broader ethic of self‑respect.
Richard Gerhart
December 18, 2025 AT 05:57Hey folks, just a heads up-if you’re using clobetasol, make sure you’re not over‑applying. Too much can thin the skin, and trust me, that’s not what you want.
Kim M
December 28, 2025 AT 07:37👀 Did you know some “big pharma” might be hiding the real cure? Stay woke! 🌐🕵️♀️
Martin Gilmore
January 7, 2026 AT 09:17Honestly-this article is a masterpiece!!! The way it breaks down the itching‑the‑immune‑battle-simply spectacular!!!
Aayush Shastri
January 17, 2026 AT 10:57Mind the itch, mind the health.
Quinn S.
January 27, 2026 AT 12:37It is imperative to note that the indiscriminate use of topical steroids without proper medical supervision may lead to iatrogenic complications, thereby contravening accepted standards of dermatological care.
Dilip Parmanand
February 6, 2026 AT 14:17Stay consistent with treatment; results follow.
Sarah Seddon
February 16, 2026 AT 15:57Let’s rally together, friends! 🌈 Imagine a world where every rash gets the love and care it deserves-our skin will thank us with sparkling confidence and radiant health!