Antacid-Antibiotic Timing Calculator
Avoid Antibiotic Failure
Antacids containing aluminum, magnesium, or calcium (like Tums, Mylanta, Maalox) can significantly reduce antibiotic absorption. This calculator shows the minimum time you should wait between taking your antibiotic and antacid to avoid treatment failure.
Recommended Timing
When you’re dealing with heartburn and an infection at the same time, it’s easy to grab an antacid like Tums or Maalox along with your antibiotic. But doing that without timing it right can make your antibiotic work less-maybe even fail completely. This isn’t just a theoretical concern. Real people have had recurring infections, failed treatments, and longer recoveries because they didn’t know antacids can block antibiotics from being absorbed.
Why Antacids Interfere with Antibiotics
Antacids work by neutralizing stomach acid using metal ions like aluminum, magnesium, and calcium. These same metals bind tightly to certain antibiotics in your gut, forming hard-to-dissolve complexes. Think of it like a magnet pulling the antibiotic away from where it needs to be absorbed. The result? Less of the drug enters your bloodstream, so it can’t fight the infection properly. This isn’t true for all antibiotics. The biggest problems happen with tetracyclines (like doxycycline) and fluoroquinolones (like ciprofloxacin and levofloxacin). Studies show tetracycline absorption can drop by 70-90% when taken with an aluminum-based antacid. Ciprofloxacin drops from 70% bioavailability to as low as 15-25% under the same conditions. That’s not a small drop-it’s enough to turn a successful treatment into a failed one. Even amoxicillin, which many assume is safe, can be affected. One study found its absorption dropped by 18-22% when taken with aluminum-magnesium antacids. Other antibiotics like diclofenac and metformin are also impacted, but antibiotics are the most dangerous because underdosing can lead to resistant infections.Which Antacids Are the Worst?
Not all antacids are created equal. The ones with aluminum hydroxide, magnesium hydroxide, or calcium carbonate are the biggest culprits. Common brands include:- Tums (calcium carbonate)
- Mylanta (aluminum hydroxide + magnesium hydroxide)
- Maalox (same as Mylanta)
- Rolaids (calcium carbonate + magnesium hydroxide)
What Happens When It Goes Wrong
A 2023 meta-analysis found that people who took antacids and antibiotics together without spacing them out had a 37% higher chance of treatment failure. That means:- Urinary tract infections didn’t clear up
- Pneumonia got worse
- Skin infections spread
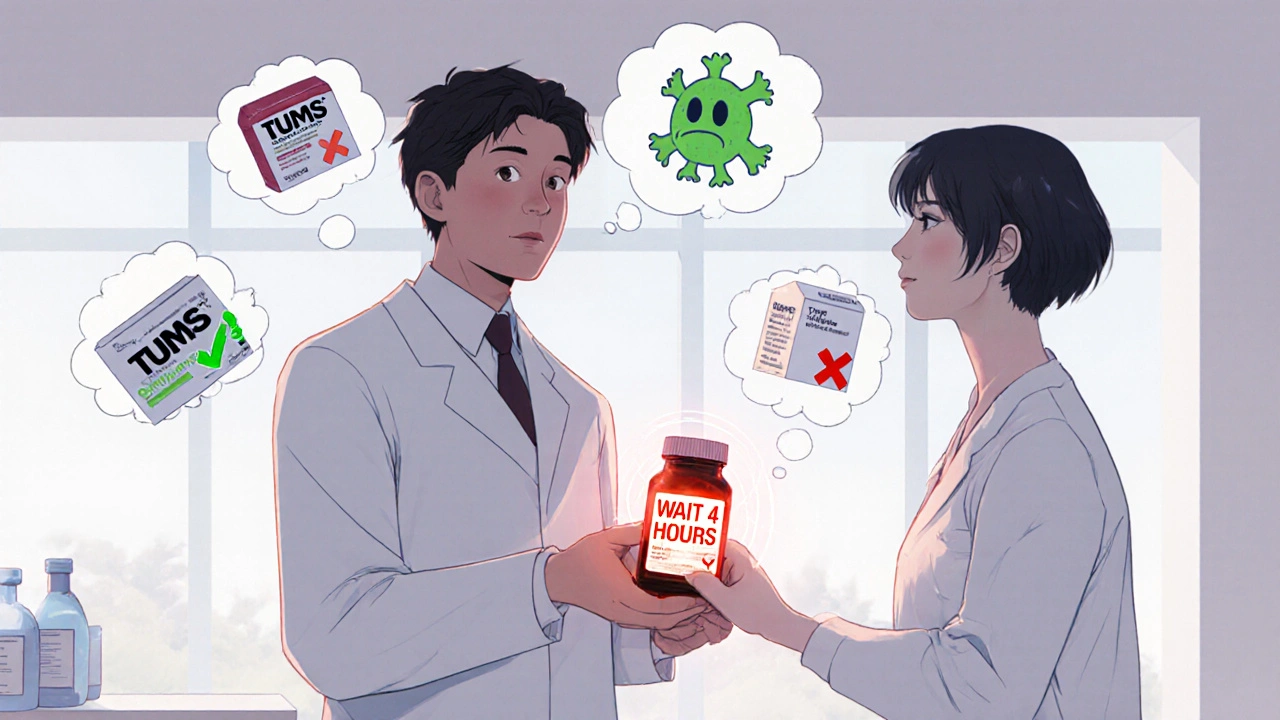
How to Fix It: Timing Matters
The solution isn’t to stop using antacids. It’s to time them right. For tetracyclines (doxycycline, minocycline):Take the antibiotic at least 2 hours before or 4 hours after the antacid. For fluoroquinolones (ciprofloxacin, levofloxacin):
Wait 4 to 6 hours between doses. These antibiotics are especially sensitive, and even a 2-hour gap might not be enough. For other antibiotics like amoxicillin or azithromycin: While the risk is lower, it’s still safest to separate them by at least 2 hours if you’re taking a strong antacid. If you’re unsure, take the antibiotic on an empty stomach (30-60 minutes before eating) and delay the antacid until after your next meal. That gives the antibiotic time to absorb before the antacid hits.
Who’s at Highest Risk?
This interaction doesn’t affect everyone equally. High-risk groups include:- Elderly patients-often on multiple medications and may not read labels
- People with chronic heartburn-who use antacids daily
- Patients on long-term antibiotics-like those treating Lyme disease or acne
- Those with kidney issues-who may have reduced ability to clear excess aluminum or magnesium
What Pharmacists and Doctors Are Doing
The American Pharmacists Association lists antacid-antibiotic interactions as the #3 most common OTC-prescription drug interaction, making up 12.7% of all reported cases. In response, the FDA updated labeling rules in 2019 requiring clearer warnings on antacid bottles. But a 2022 audit found only 67% of major brands fully complied. Pharmacists are now trained to ask: “Are you taking anything for heartburn?” before dispensing antibiotics. Many pharmacies now print warning stickers on antibiotic bottles when antacids are listed in the patient’s profile. A 2022 study showed that when patients received clear timing instructions from a pharmacist, treatment failure rates dropped by 28%. Simple education makes a huge difference.
What to Do Instead
If you need acid relief while on antibiotics, here’s what works better:- Switch to famotidine (Pepcid)-an H2 blocker. It doesn’t bind antibiotics and lasts longer.
- Use omeprazole (Prilosec OTC)-a PPI. No metal ions, so no chelation. Just wait 30-60 minutes after taking it before eating.
- Try lifestyle changes-avoid spicy food, eat smaller meals, don’t lie down after eating. These reduce the need for antacids altogether.
Why This Matters Beyond One Infection
Every time an antibiotic fails because of poor absorption, there’s a risk the bacteria survive and mutate. That’s how antibiotic resistance starts. The CDC estimates over 35,000 deaths in the U.S. each year come from infections that no longer respond to standard antibiotics. This isn’t just about one pill failing. It’s about making sure our antibiotics keep working-for you, for your family, for everyone.Quick Summary
- Antacids with aluminum, magnesium, or calcium can cut antibiotic absorption by up to 90%.
- Tetracyclines and fluoroquinolones are the most affected-never take them with antacids.
- Separate doses by at least 2-6 hours depending on the antibiotic.
- Use famotidine or omeprazole instead if you need ongoing acid relief.
- Only 32% of antacid users know about this risk-don’t assume it’s safe.
- Improper timing contributes to treatment failure and antibiotic resistance.
Can I take Tums with amoxicillin?
It’s not recommended. While amoxicillin is less affected than tetracyclines or ciprofloxacin, studies show its absorption can drop by 18-22% when taken with aluminum-magnesium antacids like Tums. To be safe, wait at least 2 hours after taking amoxicillin before taking Tums, or take Tums 4 hours after your antibiotic dose.
How long should I wait after taking an antacid before taking an antibiotic?
For tetracyclines like doxycycline, wait at least 2 hours after the antacid. For fluoroquinolones like ciprofloxacin, wait 4 to 6 hours. If you’re unsure, space them out by 4 hours. Taking the antibiotic on an empty stomach first thing in the morning, then the antacid after lunch, is a practical way to avoid overlap.
Do all antacids interfere with antibiotics?
No. Antacids with aluminum, magnesium, or calcium are the main offenders. Sodium bicarbonate (like Alka-Seltzer) has less binding power but can still affect absorption by changing stomach pH. H2 blockers (famotidine) and proton pump inhibitors (omeprazole) don’t contain metal ions and are generally safe to use with antibiotics.
What happens if I accidentally take them together?
One accidental dose is unlikely to cause major harm, especially with a short course of antibiotics. But if you do this regularly-like taking antacids daily with your antibiotic-it can lead to subtherapeutic drug levels, treatment failure, and potentially contribute to antibiotic resistance. If you’ve done this multiple times, tell your doctor. They may need to check your infection status or switch your antibiotic.
Can I use antacids while on antibiotics for a sore throat?
If you’re on amoxicillin or azithromycin for a sore throat, the risk is lower but still present. If you’re on doxycycline (sometimes used for certain throat infections), avoid antacids entirely. For safety, space them apart by at least 2 hours. If your heartburn is mild, try chewing gum or sipping water instead-it can help reduce acid without blocking your antibiotic.








Mark Kahn
November 22, 2025 AT 16:30Hey, just wanted to say this is super helpful. I had no idea Tums could mess with my antibiotics. I’ve been taking them together for years because I get heartburn after meals. I’ll start spacing them out now. Thanks for the clear info!
Anne Nylander
November 23, 2025 AT 02:01OMG this saved me!! I was on azithromycin for a chest infection and took Maalox every night because I couldn’t sleep. My doc was so confused why it wasn’t working. Now I know why. I switched to Pepcid and boom-felt better in 2 days. You’re a lifesaver!! 😊
Leo Tamisch
November 23, 2025 AT 23:16How is this even a topic? 🤔 The fact that metal ions bind to antibiotics is basic pharmacokinetics. I mean, if you didn’t know this by med school, maybe you shouldn’t be self-medicating with antacids in the first place. Also, ‘OTC’ doesn’t mean ‘safe with everything’-it means ‘you can buy it without a prescription.’ Big difference.
Daisy L
November 25, 2025 AT 03:47YEAH! This is why I HATE when people treat OTC meds like candy! You think you’re helping yourself, but you’re just feeding superbugs! 🚨 I’ve seen people take Tums with cipro like it’s a snack-then they come back in 2 weeks with a worse infection. It’s not just dumb-it’s dangerous. And no, ‘I’ve done it for years’ doesn’t make it okay!
Franck Emma
November 26, 2025 AT 13:13My doctor didn’t tell me. My pharmacist didn’t tell me. My mom told me. I’m 34. I shouldn’t have to learn this from my 68-year-old mom.
Corra Hathaway
November 27, 2025 AT 11:50Yessss!! This is why I always say: if you’re gonna pop pills, at least know what they’re doing to each other! 🙌 I used to mix everything like a chemistry experiment-now I use a little notebook and color-code my meds. Life’s better when you’re not fighting your own body. 😘
Pravin Manani
November 28, 2025 AT 15:01From a clinical pharmacology perspective, the chelation mechanism is well-documented for divalent and trivalent cations (Al³⁺, Mg²⁺, Ca²⁺) forming insoluble complexes with the carboxyl and keto groups of fluoroquinolones and tetracyclines, thereby reducing bioavailability via decreased membrane permeability and accelerated GI transit. The 70–90% reduction in AUC observed in pharmacokinetic studies is statistically significant (p < 0.001), and the clinical implication-subtherapeutic serum concentrations-is a validated risk factor for therapeutic failure and selection of resistant strains. The recommended temporal separation of 2–6 hours is empirically derived from Cmax and Tmax profiles, and while H2RAs and PPIs are preferable for chronic use, they do not eliminate the risk of altered gastric pH affecting absorption of pH-dependent antibiotics such as ketoconazole or erlotinib.
Eliza Oakes
November 30, 2025 AT 00:52Wait, so you’re telling me I can’t just take my antacid when I want? What, am I a robot now? I’ve been taking Tums with my doxycycline for months and I feel fine. Maybe the ‘studies’ are wrong. Maybe I’m just naturally resistant. Or maybe Big Pharma wants us to buy more expensive drugs. 🤷♀️
Noah Fitzsimmons
December 1, 2025 AT 12:49Oh wow. A whole article about spacing out pills. Did you also write one on ‘don’t put your phone in the microwave’? Because that one’s still relevant too. 🙃
Chris Vere
December 2, 2025 AT 18:15It’s interesting how such a simple biological interaction-metal ions binding to molecules in the gut-can have such profound consequences on public health. We treat medicine like a vending machine: insert coin, get result. But the body is not a machine. It’s a system of delicate balances. When we disrupt one part without understanding the whole, we don’t just risk failure-we risk evolution. Antibiotic resistance isn’t just a medical crisis. It’s a moral one. We owe it to future generations to use these tools with care.
Clifford Temple
December 2, 2025 AT 21:58This is why America is falling apart. People can’t even follow basic instructions. You want to take antacids? Fine. But don’t ruin the antibiotics that keep us safe. If you can’t read a label, maybe you shouldn’t be in charge of your own health. This isn’t rocket science. It’s fifth-grade science. And we’re failing at it.